Risks / Predisposing factors for developing a dry socket.
Risk factors for developing a dry socket.
While you may know that the usual cause of dry socket formation is tooth socket blood clot loss, you may not realize that certain habits, situations, and conditions, factors specifically associated with you the patient, may make this more likely to occur.
This page explains factors that tend to increase your odds of developing alveolar osteitis (a dry socket). Issues we cover include:
A – Not following your dentist’s postoperative instructions –
Possible consequences of failing to do so include directly dislodging the blood clot that’s formed in your tooth’s socket. Or, inadvisably, participating in activities or habits that may otherwise lead to its demise.
B – Having a history of previously experiencing dry sockets –
Understanding why you’ve been at risk before may help you to avoid this complication with future extractions.
C – Having undergone a difficult or surgical extraction –
Studies indicate that the higher the level of tissue trauma created during the extraction process, the greater the chances of dry socket formation. And while this may seem a risk factor beyond your control, we explain why it isn’t entirely.
D – Additional predisposing causes and risk factors.
- Smoking / Tobacco product use.
- Oral contraceptive usage (BC pills).
- Oral bacteria associated with the extraction site.
- The patient’s age. / Advanced age.
- The location of the tooth that was extracted.
Other ways to learn – Take our Dry Socket Prevention quiz that explains many of the issues you should know.
What’s to be gained by knowing about dry socket risk factors?
- Explanation and understanding – People currently suffering with a dry socket may find it to be a significant event. An understanding about predisposing factors may help them to at least understand what has transpired in their case.
- Prevention – For past or present sufferers who have additional extractions in their future, or for anyone else simply reading up and preparing for one, understanding a few basic issues, and subsequently taking steps associated with them, might play a major role in the prevention of a dry socket with their upcoming procedure.
Take our Dry Socket Causes quiz – A quick way to learn the important points from this page.
Dry socket risk factors –
A) Not following your dentist’s post-op instructions.
The blood clot that forms in your tooth’s socket following its removal plays an important role in the healing process to come, with its loss (complete or partial) being a major causative factor in the formation of dry sockets. Here’s why.
As a preventive measure, many of the items listed as do’s and don’ts in your dentist’s post-extraction instructions have to do with limiting activities and behaviors that may be detrimental to this goal. Here’s an example of some of the issues frequently addressed:
Proper blood clot formation helps to prevent dry socket formation.
1) The rolled or folded-up gauze is placed directly over the extraction site.
2) Enough gauze is placed so that when the patient closes they apply firm pressure to it.
1) Clot formation.
- Place firm biting pressure on the gauze packing that has been placed over their extraction site for the next 30 to (preferably) 60 minutes.
2) Protecting the clot from physical loss.
- Avoid vigorous rinsing or spitting.
- Refrain from creating negative-pressure situations, such as sucking on a straw, or drawing in on a cigarette.
- Minimize physical activities and exercise.
- Avoid hot liquids such as coffee and soup. (It’s thought that hot items tend to dissolve blood clots.)
Each of the factors above could place the blood clot at an increased risk of being dislodged and physically lost, and for that reason should be avoided.
How much of an issue is patient clot disruption?
▲ Section references – Blum, Kolokythas
In response, we will state that …
- We’ve read through a number of post-extraction instruction sets found on the websites of dentists and oral surgeons. And it’s our impression that the vast majority do include this consideration in their directions. (As do we, see the link below.)
- Protecting the clot from premature loss certainly seems to make sense, especially since that’s what would normally be expected to occur during socket healing. Also, it’s hard to imagine a scenario where taking this precaution would be detrimental in any way.
- However, with the lack of scientific evidence supporting this issue, it might be better categorized as a “best practice” as opposed to a major preventive factor. Either way, it’s important to note that this is something that you (the patient) have a great deal of control over.
Prevention guidelines for this risk factor.
Don’t forget, your dentist’s instructions include other directions too.
Beyond the abbreviated do’s and don’ts we’ve outlined above related to controlling bleeding and blood clot protection, your dentist should also provide you with a comprehensive list of additional postoperative directions.
They should include instructions for both the first 24 hours, and then the days beyond. As an example of what they will include, we begin our discussion of common post-extraction instructions here. See the list.
Note: A separate risk factor covered in post-op instructions that you control (and therefore can be used as a preventive measure) is smoking avoidance. Why it’s important.
B) Having a previous history of experiencing dry sockets.
If you’ve had one before, you must consider yourself at elevated risk for developing a dry socket with other extractions.
Research.
A study by Reekie (2006) followed 302 patients who had routine extractions performed by general dentists. 16 of these subjects had a history of experiencing a dry socket before.
- Out of the group of 16 participants with a previous history, 6 (37.5%) developed a dry socket.
- Of the remaining 286 subjects, only 17 (5.9%) developed this complication.
Prevention guidelines for this risk factor.
The unanswered question with the above study would simply be whether the major risk issues involved were primarily patient-related (systemic/medical issues, at-risk behaviors) and therefore likely to continue to exist. Or more so factors associated with the procedure itself (initial conditions, the way in which the procedure was performed, etc…) which might vary between surgeries.
Either way, as a patient, the factors you control the most are those associated with your dentist’s list of postoperative instructions. So especially when a previous history of experiencing dry sockets exists, strictly adhering to proper post-extraction protocol should always be considered of paramount importance and your best chance of lowering your risks.
C) Trauma associated with difficult or surgical tooth extractions.
▲ Section references – Noroozi, Kolokythas
As examples:
- A review of published literature by Torres-Largares determined that surgical tooth extractions (such as the case where an impacted wisdom tooth is removed), as opposed to non-surgical ones (no tissue flap raised, no bone removal), resulted in a ten-fold increase in the incidence of dry socket. Learn about Surgical Extractions.
- Blondeau monitored the postoperative healing of 550 patients who had impacted lower wisdom teeth extracted. The study reported that 92% of cases that subsequently developed a dry socket involved surgical procedures where bone tissue had been trimmed.
▲ Section references – Torres-Largares, Blondeau
Why the greater risk?
Several theories have been suggested as an explanation of this relationship. They include:
- Difficult extractions may result in the compression of the bony walls of the tooth’s socket and also cause blood vessel thrombosis (the formation of a blood clot in a vessel), with both interfering with blood perfusion (flow) and thus the formation of an adequate blood clot.
Or, since difficult extractions often involve older denser (less vascular) bone, a lack of perfusion into the socket may be the norm.
- Some theories suggest that the above lack of perfusion results in delayed healing, and therefore decreased resistance of the wound’s tissues to infection.
- Trauma created during the extraction process may cause inflammation of the bony socket, which subsequently triggers the release of compounds that cause blood clot lysis (disintegration). More traumatic surgeries are thought to result in higher levels of these compounds.
This explanation also includes the theory that additional compounds that stimulate nerve pain receptors (kinins) are also released during this reaction, thus explaining why dry sockets can be so painful.
▲ Section references – Bowe, Cardoso, Kolokythas
Will your dentist know what level of surgical trauma will be involved?
Yes, they should have some relative expectations. And, in fact, developing an opinion is an important part of their planning your extraction. That’s because their ability to correctly interpret the challenge that a tooth will pose beforehand will influence the way its removal is initially approached.
For example, attempting to remove a tooth conventionally when a surgical approach is really needed only serves to increase the level of trauma associated with the procedure, and thus the patient’s potential for developing a dry socket.
Examples of the level of surgical trauma that an extraction might pose.
A correlation exists between extraction difficulty and the risk of dry socket formation.
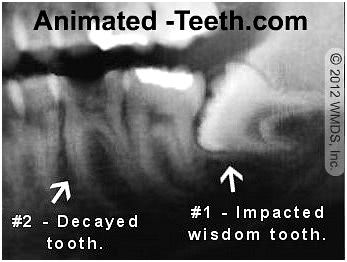
Both of these extractions offer challenges due to the tooth’s condition or positioning.
- Make an incision through the gum tissue and reflect it back (create a “flap”) so the bone covering the impacted tooth can be accessed.
- Trim away a portion of the bone that lies over the tooth, so it, in turn, can be accessed.
- Section the tooth (cut it into pieces), and then remove each piece through the opening that’s been created.
Of these steps, creating the tissue flap and trimming bone are events that create a higher level of surgical trauma than that associated with routine extractions.
And because of their need, this surgical site can be expected to be at a relatively greater risk for developing a dry socket.
Example #2 – In comparison, when the decayed tooth (tooth #2 in our picture) is removed, there’s a good chance that far less tissue manipulation will be required. The dentist already has direct access to the tooth, so it’s likely that no gum or bone trimming will be required.
That means when compared to our first example, extracting this second tooth should result in less surgical trauma. And that means that the patient’s risk for dry socket formation in this location would be expected to be less too.
Example #3 – For this example, we’ll continue our discussion about removing tooth #2 in the picture above, and how an unexpected traumatic extraction might come about.
The scenario might be one where the extent of the decay is greater than anticipated. And as a result, the tooth breaks, leaving behind a root fragment that simply can’t be retrieved conventionally.
What will be needed is some type of surgical intervention, in the sense that now some bone will need to be removed (so the broken portion can be accessed), and maybe even a flap laid (to aid with accessing and removing bone).
The consequences.
If that’s what’s needed, fine. But the question at hand would be, did the two-phase procedure (failed and then successful attempts at removal) collectively create more procedure trauma, and therefore create a greater risk of dry socket formation, than if a surgical extraction was performed at the start? (This is an issue we’ll continue discussing below.)
Prevention guidelines for this risk factor.
a) Patient cooperation.
As a patient, you might think that there’s little you can do to reduce the levels of difficulty of an extraction. On the contrary, however, there’s a great deal you can do. It’s referred to as patient cooperation.
Make it your goal to be as good of a patient for your dentist as possible so they can focus their attention on performing their tasks, rather than managing you.
That difference might mean that they can remove a difficult tooth comparatively less traumatically. And as a result, help to set the conditions where it is less likely that you’ll have a dry socket.
b) Operator experience is important.
This risk factor is why we included Example #3 above (the situation where what was thought would be a simple extraction turned into a surgical one). We were trying to point out how having a less-experienced/less-skilled dentist remove your tooth may place you at greater risk of having a dry socket.
This phenomenon is generally considered confirmed by research (Kolokythas, Cardoso) [linked above]. As an example:
- Oginni followed the healing outcome of over 3000 extraction cases (encompassing all types and levels of difficulty) that were performed at a teaching hospital.
- 70% of the cases that experienced a dry socket were performed by students.
As an explanation:
- A more experienced operator may be able to tease a tooth out of its socket less traumatically than those with less experience or skill. Also, surgical time, which correlates with the level of surgical trauma created, is likely to be shorter with more experienced clinicians.
- A more experienced dentist may be more likely to recognize a challenging situation initially.
That’s favorable because a planned surgical extraction will likely result in less total tissue trauma than the situation where complications have cropped up and it is needed as an additional step (Example #3 above).
Choosing between a dentist vs. an oral surgeon.
In general, this risk factor means that you should ask your dentist questions. It’s their obligation to be forthright with you about their ability to perform a procedure in a fashion that reasonably approaches the level of skill and competence of other practitioners in your area, including specialists. If they can’t, a referral might be indicated.
D) Additional risk factors for dry socket formation.
The remainder of this page covers the following issues that may put you at greater risk for developing alveolar osteitis (a dry socket) following your extraction.
- 1) Smoking / Tobacco use.
- 2) Oral contraceptive use.
- 3) Oral bacteria associated with the extraction site.
- 4) Advanced patient age.
- 5) The location of the extracted tooth.
1) Smoking.
Studies have consistently found that smokers are significantly more prone to dry socket formation, as opposed to extraction patients who don’t. (Bowe)
As an example, a frequently cited historic study (Sweet) evaluated the healing outcome of 400 patients who had lower wisdom teeth removed. Within this population, it was found that:
- Patients who smoked 10 cigarettes per day (half a pack) experienced a greater than fourfold increase in the incidence of dry socket formation (12% vs 2.6%).
- The incidence rate for patients who smoked 20 cigarettes (one pack) daily was higher yet at 20%.
- Smokers who smoked on the day of their surgery, or within 24 hours following their procedure, experienced a 40% incidence rate for this complication. (Remember, that’s in comparison to a 2.6% rate for the non-smoking portion of this study’s subjects.)
▲ Section references – Bowe, Sweet
Why does smoking cause dry sockets?
The precise cause-and-effect relationship between smoking and alveolar osteitis has yet to be definitively determined. However, the following explanations have been proposed. They seem to fall into two categories: 1) Effects on the blood clot that forms in the tooth’s socket and 2) Inhibiting the body’s normal healing process.

Refraining from smoking after an extraction can help to prevent dry socket formation.
- The negative-pressure sucking action of smoking may dislodge or disrupt the blood clot that’s formed in the tooth’s socket. Or the hot gases themselves may have a compromising effect on it.
- Several studies have found that the sockets of smokers don’t fill in with blood as readily after an extraction, thus leading to sub-par clot formation.
This effect is in part blamed on nicotine, which triggers vasoconstriction. (A constriction of blood vessels, which leads to reduced blood flow).
- As a person smokes, the carbon monoxide that enters their bloodstream combines with blood cell hemoglobin more readily than oxygen.
This effect serves to reduce the amount of oxygen that can be carried to, and therefore is available for, their extraction site’s healing tissues.
- Nicotine creates other effects that tend to interfere with the normal healing process, ranging from inhibiting the production of compounds needed for tissue repair to affecting the proliferation of types of cells that play important roles in the healing process.
- At a local level, direct exposure to tobacco smoke may damage or be toxic to cells.
▲ Section references – Ozkan, Kolokythas, Meechan, Sweet
Prevention guidelines.
▲ Section references – Bowe
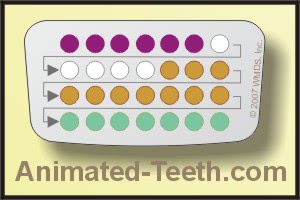
2) Oral contraceptives (BC pills).
Studies suggest that women who take birth control pills are at greater risk for developing a dry socket. For example:
- A study by Garcia followed 267 women following their lower wisdom tooth extractions. 87 of these subjects were currently taking oral contraceptives.
- 11% of women in the oral-contraceptive group developed a dry socket. Of the remaining subjects, only 4% experienced one.
Background
An interesting backstory associated with this risk factor is its history.
- Up until the 1960s, it was generally considered that the incidence of dry socket formation was similar for both men and women. From this decade on, however, this statistic was found to have changed. The assumption is that the shift was due to the increased use of birth control pills that began at that time.
- This factor may have been more of an issue during those earlier decades when oral contraceptives were formulated with a larger dosing of the hormone estrogen than they are nowadays.
▲ Section references – Bowe
Why does taking oral contraceptives increase the risk of dry sockets?
▲ Section references – Noroozi
Prevention guidelines for this risk factor.
Planning the timing of your extraction may help.
Women who take birth control pills may be able to lessen their risks by scheduling their tooth extraction during those days when the estrogen dosing of their contraceptive regimen is at its lowest.
▲ Section references – Cardoso
3) Oral bacteria.
The theory that bacteria play a role in dry socket formation has been postulated for a long time. But as of yet, no definitive cause and effect (such as the identification of specific micro-organisms) has been proven.
Identified risk factors.
This theory stems from reports where the following factors and issues have been found to be associated with an increased risk of dry socket formation.
- Poor patient oral hygiene practices.
- A high bacterial count (anaerobic bacteria in particular) in the region of the extraction site, either before or after the patient’s procedure.
- A pre-extraction infection has been associated with the tooth. This includes gum disease (periodontitis), infection in tissues that surround the tooth (such as pericoronitis), or periapical infection (infection associated with necrotic nerve tissue inside the tooth).
▲ Section references – Blum, Bowe
Prevention guidelines for this risk factor.
As a part of investigating these observations, studies have suggested that the following steps may be useful in helping to prevent dry sockets:
- Have the patient rinse with an antibacterial mouthwash (such as chlorhexidine, a prescription product) before their procedure is performed.
- Starting the patient on systemic antibiotics (usually oral) prior to their procedure.
- Placing an antibacterial or antibiotic-impregnated packing into the socket immediately following the tooth’s removal.
▲ Section references – Daly, Bowe
Dry sockets are not usually treated with antibiotics.
Despite whatever role oral bacteria may play in causing them, protocols for treating dry sockets typically do not include the routine use of systemic antibiotics. (Bowe) How dentists treat dry sockets.
▲ Section references – Bowe
4) Patient age.
Several studies have found a correlation between patient age and the formation of dry sockets. However, there’s been a lack of agreement about precisely which age group is at greatest risk.
- It seems this complication is rarely a problem during childhood, or even for patients up to the age of 20 years.
- Possibly a person’s risk peaks in their 30’s and 40’s.
▲ Section references – Bowe, Noroozi
As a rule of thumb, it seems safe enough to say that relatively younger patients are generally at less risk than comparatively older ones. (This is one reason why dentists usually suggest that a patient should have their wisdom teeth removed during their late teens or early 20’s. Wisdom teeth age considerations.)
Why does this correlation exist?
As an explanation, it’s frequently pointed out that relatively older patients tend to have increased jawbone density. And with cases involving wisdom tooth removal, more complete root development. Both of these factors can increase procedure difficulty, and therefore the potential for surgical trauma (a known risk factor).
Additionally, comparatively older people generally have a relatively reduced capacity for healing. And may be more likely to be smokers (a known risk factor).
Prevention guidelines for this risk factor.
- Following your dentist’s postoperative instructions as closely as possible is always a good idea and should help to reduce your risks.
- With wisdom teeth, if you’re in the ideal age group for their removal and your dentist has made a satisfactory case in favor of it, give their proposal serious consideration.
5) Tooth location.
A patient’s risk for developing a dry socket has been shown to correlate with the location of the tooth being extracted. As examples:
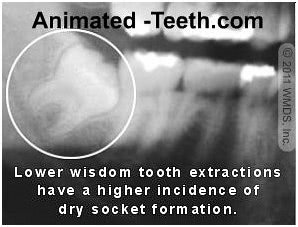
Lower impacted wisdom tooth extractions tend to have the highest risk for dry socket formation.
- Having a back tooth pulled (especially a molar) tends to pose a greater risk than when front teeth are removed.
- The risk is 10 times higher when a lower tooth is extracted as opposed to an upper one.
- The greatest level of risk for dry socket formation is with impacted lower wisdom tooth extractions (see picture). The incidence rate for these surgeries has been reported to be as high as 45%.
- As a point of curiosity, a study by Nusair found a higher incidence of dry sockets with single-tooth extractions vs. multiple ones (7.3% vs 3.4%).
▲ Section references – Nusair, Cardoso
Why this relationship?
The characteristics of the bone that surrounds teeth in different areas of the mouth vary, most notably upper vs. lower jaw. By nature, the bone tissue of the lower jaw is denser and less vascular than that of the upper, and for that reason may have a less robust healing capacity.
▲ Section references – Kolokythas
Prevention guidelines for this risk factor.
If the location/positioning of your tooth is one that places you at greater risk for a dry socket, as preventive measures you can:
- Make sure to follow your dentist’s post-op instructions as closely as possible.
- If your extraction is surgical in nature, choosing a practitioner whose skill level and expertise are commensurate with your procedure (for example, choosing an oral surgeon vs. a dentist Pros and cons.) can help to minimize your risks.
Page references sources:
Blondeau F, et al. Extraction of impacted mandibular third molars: postoperative complications and their risk factors.
Blum IR. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review.
Bowe DC, et al. The management of dry socket/alveolar osteitis.
Cardoso CL, et al. Clinical concepts of dry socket.
Daly B, et al. Local interventions for the management of alveolar osteitis (dry socket).
Garcia AG, et al. Does oral contraceptive use affect the incidence of complications after extraction of a mandibular third molar?
Kolokythas A, et al. Alveolar Osteitis: A Comprehensive Review of Concepts and Controversies
Meechan JG, et al. The effect of smoking on immediate post-extraction socket filling with blood and on the incidence of painful socket.
Noroozi AR, et al. Modern concepts in understanding and management of the “dry socket” syndrome: comprehensive review of the literature.
Nusair YM, et al. Prevalence, clinical picture, and risk factors of dry socket in a Jordanian dental teaching center.
Oginni FO, et al. A clinical evaluation of dry socket in a Nigerian teaching hospital.
Ozkan A, et al. The Effect of Cigarette Smoking on the Healing of Extraction Sockets: An Immunohistochemical Study.
Reekie D, et al. The prevention of ‘dry socket’ with topical metronidazole in general dental practice.
Sweet JB, et al. The relationship of smoking to localized osteitis.
Torres-Largares D, et al. Update on dry socket: a review of the literature.
All reference sources for topic Dry Sockets.