How to know if your tooth needs root canal.
Does your tooth need root canal?
Figuring out if a tooth requires endodontic therapy isn’t always a straightforward or easy task.
As we outline and explain on this page, there are a number of characteristic signs and symptoms that people, whose tooth does need treatment, frequently do experience. And there are also additional, sometimes less obvious, ones that your dentist knows to look for.
A diagnosis must be based on a complete picture.
But while the symptoms and clinical signs discussed on this page are indicative of teeth that require treatment, they’re not diagnostic on their own.
A final determination about your tooth’s need for root canal therapy can only come from your dentist. And then only after their collecting information from all available sources (including x-ray evaluation What they look for. and clinical testing of your tooth How they test.), and evaluating it collectively.
So have a good read with this page. We hope it’s informative for you. But bottom line, if you can correlate issues we discuss on this page with your suspected tooth, you shouldn’t delay in reporting to your dentist so they can evaluate your situation fully.
COVID-19 / Treatment access considerations.
Due to the 2020 Coronavirus pandemic, many patients will find that their dentist’s office does not currently keep regular office hours.
Some level of care should still be available.
In the case that you find yourself in need of assistance with a tooth that seems to display signs of endodontic pathology (a root canal-related problem), don’t overlook the fact that most dental offices should still be offering some level of emergency care for patients of record, and possibly new patients too.
Alternatives.
There aren’t any home remedies that can provide definitive care for a tooth that has endodontic problems. Direct treatment from a dentist is required.
However, in regard to obtaining pain relief, and beyond what might be tried intuitively, this remedy may work First Aid with teeth poised at a specific stage of their syndrome. For other cases, however, immediate relief may only be possible via treatment performed by a dentist.
A common method of managing endodontic cases.
In situations where the direct care of a dentist is not possible, some cases can be managed via the use of prescription medications. Definitive treatment is then provided for the tooth at a later date.
Depending on the specifics of the case, an antibiotic is often prescribed in an attempt to limit/control the tooth’s associated infection. Since it may take some days to accomplish its effect, a prescription pain reliever is often prescribed too.
A phone consultation with your dentist may be all that’s needed to implement this approach (for cases where they feel it’s appropriate). Similarly, a physician at an emergency-care facility could initiate this same interim plan.
Signs and symptoms of needing root canal treatment.
- Symptoms you have noticed. What to look for. – It’s frequently the appearance of pain, or signs of infection and/or swelling, that first signal to a person that their tooth has a problem.
Your dentist will quiz you about your perception of the symptoms you’ve noticed: Type, location, onset, triggers, duration, what if anything provides relief. Their evaluation will then involve trying to confirm, and possibly even reproduce, what you have reported.
- Clinical signs possibly only obvious to your dentist. What they look for. – Some teeth seem to give little indication that there’s a problem within their nerve space. But to the trained eye, they may be displaying subtle signs that hint that a problem likely exists.
Common tip-offs: Individually darkened teeth, evidence of infection or drainage from it, soft tissue changes.
- Additional evaluation. – As mentioned above, once the signs you have noticed have been evaluated by your dentists, and possibly confirmed by the additional ones they know to look for, they’ll further their investigation with clinical testing of your tooth and x-ray evaluation. (See links above to our pages that discuss these issues in detail.)
FYI – Since performing endodontic therapy is the needed solution for such a wide variety of problems (acutely inflamed teeth, teeth with dying or dead nerve tissue, cracked teeth, failed initial root canal treatment, etc…), there isn’t just a single set of symptoms that appears in every case where it’s needed.
It’s only after sorting through all of the bits of information they’ve collected, from all available sources, that your dentist can then determine if root canal, or possibly an entirely different dental procedure, seems to be the appropriate solution.
In some cases, the data that’s been collected may be inconclusive or even conflicting. If so, the patient may need to wait and be reassessed at a later time, or be referred to a specialist endodontist for evaluation.
1) Root canal signs and symptoms that you (the patient) may notice.
Probably the set of symptoms that are most associated (and feared) by patients as a sign that root canal treatment is needed for their tooth are those that occur during an acute tooth flare-up. (In dental terms, referred to as an “acute apical abscess.”)
Acute apical abscess –
- A quick onset.
- Spontaneous pain – pain the occurs on its own, unprovoked.
- Extreme tenderness of the tooth to pressure – like to biting or tapping on it.
- Swelling of associated soft tissues – a sign of the spread of pus from the tooth’s infection.
Despite what a person might fear or be inclined to expect, with many if not most cases, just one or a few of these types of symptoms will be experienced. And possibly then, only vaguely.
Also, with some cases additional or even entirely different signs may be the ones noticed. That’s because what exactly a person does experience will simply depend on the state of pathology that currently exists with the tooth’s nerve/nerve space, and that can be quite varied.
For our discussion about what types of signs or symptoms might be noticed, we’ve addressed each category individually.
a) Pain.
Type of pain.
- The discomfort can range from sharp and intense to a dull ache. Its level may range from slight to extreme.
Characteristically:
- The pain may include a throbbing component (feels like it has its own heartbeat).
- Its character may change (lessen or intensify) as you change your posture (stand up, bend over, lie down, etc…).
- The discomfort may be severe enough that it wakes you when sleeping.
Onset and duration.
- Depending on how long the underlying condition has existed, some level of discomfort may have presented itself intermittently before (previous days, weeks, months). In other cases, this will be the person’s first painful experience.
- The pain may be spontaneous (hurts on its own, unprovoked) or only triggered in response to a stimulus.
- In cases where the pain is spontaneous, it may be intermittent or continuous.
- If a triggering event is involved, it may be: Chewing or biting pressure, the pressure of pressing or tapping on the tooth, thermal insult (like exposure to hot or cold foods and beverages), sweets.
Once the triggering stimulus has been removed, rather than disappearing immediately the discomfort frequently lingers (often for 30 seconds or longer). It may then finally fade away, or continue for an extended period of time.
In some cases, heat application will bother the culprit tooth and cold liquids or ice will settle it down. (Ice application is sometimes used by patients to provide temporary relief.)
- It’s common that over-the-counter analgesics (pain relievers) are ineffective in controlling the pain.
Location.
- It may be quite easy for the patient to identify which tooth hurts. At other times the discomfort may be vague and nondescript.
- The person may be able to tell which general area is painful but not which tooth.
- The pain may be referred, meaning that the tooth or area that hurts the most is not the one that is the actual source of the problem.
▲ Section references – Germain, Iqbal, Bender
Remember, pain isn’t always a sign that root canal is needed.
While each of the above scenarios may be an indication that root canal treatment is needed, there simply isn’t a single set of signs that appear in every case that foretell for sure that it is. In fact, many of the symptoms above can also be an indication of more benign tooth conditions.
Beyond just quizzing you about what you have experienced, your dentist may also try to reproduce events that trigger your discomfort so they can evaluate what you are experiencing first hand. (See “testing” section below.)
Even then, while they may have formed a strong opinion about your tooth’s condition, they’ll still wait until they have collected other information before making a final diagnosis.
So, if you experience some type of pain, be concerned and proceed with seeking assistance. But in regard to it absolutely being a sign that you need root canal, there can be other explanations.
Other dental conditions that may cause tooth pain.
As a part of their differential diagnosis, your dentist will consider additional conditions that may be the cause of your tooth’s discomfort. They can include:
- Tooth decay, tooth fracture, a defective, deep, extensive or new dental restoration, sinus infection, tooth clenching and grinding (bruxism), periodontal (gum) disease, exposed dentin.
If any of these are identified, the dentist will likely initiate treatment aimed at both managing that problem and helping the irritated tooth to settle down. If it doesn’t respond positively, or if reevaluation at a later date identifies the need, root canal may still be required.
b) Gum tenderness, swelling, infection.

The abscess that forms may create obvious facial swelling.
Degree of enlargement.
- The swelling may take the form of a reddish, slightly tender, otherwise relatively normal looking area inside your mouth adjacent to your tooth.
Or, at the other extreme, appear as a localized lump or even a widely distributed area of fullness that’s noticeable in your face or possibly even your neck.
Location.
- Usually, there’s a general relationship between the location of the swelling and culprit tooth. Although, it’s possible for pus/swelling to travel or extend some distance from the source of its infection. The swelling will occur on the same side of your body as the infected tooth.
- With intraoral (inside the mouth) swelling that’s relatively minor and localized, the area of enlargement usually lies at a level that approximates the tip of the problem tooth’s root.
- Instead of pronounced swelling, a pimple-like drain for pus may form on your gums (a “gum boil”). We discuss this phenomenon more fully below.
Onset.
- The swelling may come and go as days, weeks or even months pass, possibly never disappearing completely.
- It may have presented itself for the first time, with a slow or rapid onset.
Associated symptoms.
- Swelling may be but isn’t always accompanied by the presence of pain. (The pressure associated with the buildup of pus is often what is causing the person’s tooth pain.)
- The area of swelling is characteristically tender to palpation (touch).
- Lymph nodes (like in your neck or under your jaw, on the same side as the infected tooth) may be enlarged or tender.
- If the pus causing the swelling finds a way to vent off (drain), you may notice a bad taste in your mouth. Draining pus can also be the source of foul breath odor.
- It’s possible that due to infection the tooth feels slightly elevated. (Seems as though it’s been pushed out of its socket some and is taller than its neighboring teeth.)
- To a minor extent, the tooth may also feel slightly more mobile than previously.
▲ Section references – Tronstad
Swelling isn’t always a sign that root canal treatment is needed.
Experiencing swelling doesn’t necessarily mean that you have a tooth that needs endodontic therapy but it does indicate that something is wrong somewhere and it’s presence should be taken seriously. (While rare, in extreme cases it can become so pronounced as to interfere with your ability to breathe.)
It’s a simple matter to contact your dentist’s office and report what you have experienced. They can then make a decision about what level of attention you require.
When swelling is present a dentist will frequently have their patient start a regimen of oral antibiotics. Since they typically take about 24 hours to have an effect, when you call your dentist even if they don’t feel that you need immediate examination, they may go ahead and prescribe antibiotics for you so you can get started with them.
Ways to distinguish the likely source of your swelling.
In cases where an area of tenderness and swelling is fairly small, the following rules of thumb tend to apply.
- If caused by periodontal (gum) issues, the area is often located alongside of the tooth or right at its gum line.
- When caused by an infection inside a tooth, it’s often centered in the region that approximates the tooth’s root tip.
Other dental conditions that may cause swelling.
Your dentist will consider other possible sources of infection during their examination. They can include:
- Periodontal (gum) disease, pericoronitis (most commonly associated with erupting wisdom teeth.
Whatever the source, a dentist will first take steps to manage the swelling so it doesn’t get out of hand. Then at a later point diagnose the actual underlying problem and determine what treatment is required to resolve it.
c) Additional signs.
Malaise (a general feeling of illness or uneasiness) or even fever are possible symptoms that may present themselves when a person has a tooth that requires endodontic therapy.
However, these symptoms on their own are generally considered to be just secondary in nature. (They provide no information about which tooth lies at fault, or the underlying nature of its condition.) Other signs will be weighed much more heavily by your dentist when formulating their diagnosis.
d) Frequency of symptoms.
It bears repeating that any of the signs and symptoms discussed above may involve an extended time frame. If so, they may be:
- Transient – Meaning they come and go on a day-to-day or month-to-month basis, or any frequency rate in between.
- Persistent and continual. – While possibly not always especially noticeable or intense, the symptoms never totally disappear.
So now you know. What you may experience can be incredibly varied.
By this point on this page, it should be apparent to you why a dentist’s level of experience and knowledge is so important in their being able to accurately diagnose their patient’s condition.
The range and degree of symptoms possible with root canal cases are so varied and great that there’s nothing simple about interpreting them.
To recap some examples, all of which are resolved via the exact same treatment process (performing root canal treatment):
- With low-grade chronic (long existing) conditions, the patient may experience essentially no symptoms at all.
- At the other extreme, with acute apical abscess cases, rapid onset, spontaneous (possibly severe) pain, pronounced tissue swelling, and extreme sensitivity to pressure (tapping or biting on the tooth) are all likely to be experienced.
- And of course with all other endodontic cases, what’s experienced can be essentially anything in between.
So if you do notice the kinds of symptoms discussed above, you don’t necessarily have to assume the worst. But they are an indication that your most prudent move is to be checked out by your dentist promptly.
2) Clinical signs of needing root canal that may only be obvious to your dentist.
- It’s possible (and even common) for this process to occur without producing any noticeable symptoms at all.
- In many cases, the original events surrounding the nerve’s death may have been so mild, or taken place so long ago, that they’re not remembered.
With either situation, it may take your dentist’s keen eye during their examination to discover that unbeknownst to you, your tooth requires endodontic therapy.
a) Minor signs of swelling or inflammation.
Your dentist will look for signs of infection you may have not noticed. The inspection method they’ll use is termed “palpation,” which simply means examination by touch.
Signs you might have overlooked can include areas of tenderness, hardness, fluctuation (fluid-filled tissues), crepitation (areas that make a crackling noise when pressed), and slight tissue enlargement.
They’ll use their fingers and feel alongside of the tooth in question. And compare what they feel, and your response to it, to areas involving neighboring teeth or even the same area on the other side of your mouth.
▲ Section references – Tronstad
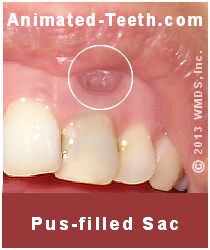
The surface opening of a sinus tract.
b) Recurring or persistent gum boils.
Patients often refer to these lesions as “gum boils.” Dentists sometimes use the term “fistulous tracts” but most accurately they are referred to as “sinus tracts.”
Why do they form?
These lesions are literally drains for pus. Instead of it building up inside the bone tissue around your tooth’s root, or in adjacent soft tissues, the tract provides a way for it to vent off totally (into your mouth).
▲ Section references – Tronstad
A gum boil may go unnoticed.
In cases where the infection inside a tooth remains low-grade, the boil will tend to be small and only have minimal taste coming from it. If so, it’s possible for a person to be totally unaware that it’s there.
Other dental conditions that may result in a sinus tract.
This type of lesion is proof positive that a problem exists but not necessarily that root canal treatment is the needed solution. For example, it’s possible that the source of the infection is a periodontal (gum disease) issue.
c) Individually darkened teeth.
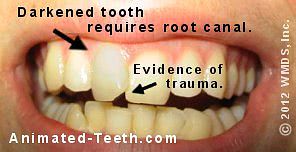
The dark color of this tooth suggests that it needs treatment.
This type of color mismatch is frequently the sole reason why a dentist will suspect that a tooth has a problem and requires root canal therapy.
Things to know.
- This phenomenon is fairly common with teeth that have experienced some type of trauma (like being banged up in an accident).
- When it occurs, the tooth may take on a dark yellow, gray or even black tint. (Here’s why the darkening occurs. Pictures | Diagrams)
- It may take place even some years (even a decade or more) after the original event occurred.
- The darkening process may not be associated with any noticeable symptoms (pain or swelling).
▲ Section references – Ingle
Having a tooth darken doesn’t always mean that root canal is needed.
This is, yet again, another sign that by itself does not necessarily mean that root canal therapy is required.
- This same type of discoloration may take place with teeth that have already had successful endodontic treatment. Or it may indicate that some nerve-space changes have occurred but at this point no attention is necessary.
- In other instances, the discoloration may be due to the presence of decay, a deteriorated filling or staining caused by a metal filling.
The color mismatch will remain.
Even after root canal therapy has been completed, the tooth’s staining will remain.
- If after the completion of the tooth’s treatment it requires a dental crown What decides?, then the placement of that restoration can be used to remedy the color mismatch.
- If not, then whitening treatments tooth bleaching may be able to provide a suitable solution.
d) Tooth mobility.
Teeth that have pulpal pathology may display increased mobility (tooth looseness). But evaluating this issue alone is typically not very diagnostic. That’s because other tooth conditions (gum disease, adaptation to the pressure of teeth grinding) can cause increased mobility too.
In making a distinction, if only one tooth seems loose, the cause may be an endodontic one. But if multiple teeth are involved, other causes are more likely involved.

If nerve exposure occurs, endodontic therapy may be needed.
e) Exposure of the tooth’s nerve.
- It’s your dentist’s obligation to notify you that this event has occurred. (Since you’ve been numbed up for your procedure, you probably won’t feel it when it happens.)
- They’ll also need to explain to you if as a result of this event your tooth now requires root canal therapy.
What’s the nerve’s outlook?
With healthy nerves.
The occurrence of the exposure and its associated events may be enough to trigger pulp tissue degeneration and the tooth’s ultimate need for root canal treatment. However, in situations where the tooth’s pulp tissue was healthy at the time of the exposure, the success of a repair made by your dentist may approach 90%. (Tronstad)
With inflamed nerve tissue.
A tooth’s potential for recovery is greatly reduced if it’s pulp tissue is already inflamed at the time of the exposure (falling to a 30 to 40% chance of success). Unfortunately, this is the usual status of teeth having advanced tooth decay. (Tronstad)
Treatment.
Based on the dentist’s interpretation of the pulp’s status (a factor they can never be 100% certain of because pulpal inflammation is typically asymptomatic), if an exposure has occurred they may feel they must advise their patient that it’s best to go ahead and plan to perform root canal treatment now (a judgment call on their part), so to avoid complications later on. (Such as the patient experiencing a painful tooth abscess, or the tooth’s root canal system undergoing calcification and as a result becoming more difficult to treat).
In cases where a repair is attempted, typically by placing calcium hydroxide paste over the wound (a process termed “pulp capping”) and then completing the tooth’s restoration, its status should be monitored periodically for some years (examination including x-rays).
▲ Section references – Tronstad
Pulp tissue exposures may be planned or unplanned.
a) Unplanned
In most cases, an exposure is an unavoidable, undesired side effect that has occurred as a dentist attempts to repair a cavity. Often one that ideally should have been treated months or years previously.
b) Planned
In a minority of cases (most of which probably involve dental crown or bridge placement), the exposure may be anticipated due to the amount of tooth structure that’s expected to need to be trimmed away so to accommodate the new dental work.
Of these two scenarios, the “unplanned” one is the case where pulp tissue inflammation is more likely not to be an issue, and therefore the success of a repair more likely. But whether pulp capping or immediately proceeding with root canal treatment makes the better plan, would simply be a judgment call made by the dentist.
What should you do if you suspect that your tooth needs root canal therapy?
Don’t delay.
If you notice any of the signs and symptoms mentioned on this page, you should establish contact with your dentist’s office and make arrangements to be evaluated and receive treatment in a time frame that they determine is warranted.
Teeth that do require endodontic therapy can be unpredictable, with the consequences of a flare-up (pain, swelling, etc…) possibly being severe.
Don’t make assumptions.
Making a misdiagnosis about their tooth’s status (by way of using website information like this) may deter some people from seeking treatment during that stage when another (simpler, cheaper and easier) repair might have been possible.
That’s because some people won’t seek treatment promptly if in their mind they think it’s already too late, will cost too much money or else the idea of having root canal is too unnerving for them.
Don’t make this mistake. If you have a tooth that’s displaying symptoms, have your dentist evaluate it sooner rather than later. Doing so may make a big difference in what you experience, what type of treatment you require and its total cost.
If root canal treatment is needed …
In the case where you do have a tooth that seemingly requires endodontic therapy, there’s not a lot, unfortunately, that you can do on your own.
The following video explains what takes place during root canal treatment. It should be obvious to anyone that only a dentist can provide this type of service, so be in touch with yours promptly.
Section highlights as a video –
Note: Dental-Picture-Show’s content and videos have now been absorbed into Animated-Teeth.com.
Things you might try …
In case you find yourself on your own for a while, there are some things you can try to help to alleviate your symptoms, at least to some degree.
- It only makes sense to discontinue any activities that tend to set your tooth off (biting on it, exposing it to hot or cold foods and beverages, etc…).
- Within the guidelines of the product you choose, you may find that using an OTC pain reliever provides some degree of relief. However, in severe cases OTC products are typically ineffective.
Placing an aspirin on the gums next to your tooth makes a poor choice. An aspirin pill (acetylsalicylic acid) is intended to be a systemic drug (absorbed internally after being swallowed), not a topical one (absorbed through the skin). Placing an aspirin next to your tooth will be ineffective in controlling your tooth’s pain and will cause a chemical burn on your gum tissue.
- Sometimes being placed on an antibiotic (and sooner rather than later, see above) can be a big help in limiting what you have to endure. And although a prescription is required, just a phone call to your dentist may be enough to get the ball rolling towards your obtaining one.
- Since all dentists know that emergencies do happen, they’ve probably made some type of plan for when their patients experience them. You should call your dentist’s office to see if there’s a message describing the type of assistance they have to offer.
Home remedy: Try placing ice on your tooth.
In some cases where root canal therapy is needed, during that stage when a tooth has started to produce extended periods of constant pain, chilling it by way of holding a chip of ice, or cold liquid (ice water), against it may provide relief.
This won’t work in all cases and in fact may irritate your tooth in some. So, ease into this remedy with testing. But when this solution does work, it can provide much-needed relief until you can receive the treatment you require from your dentist.
FYI – It’s not uncommon for a dentist to have a patient arrive for emergency treatment who has with them a mug of ice water from which they sip at regular intervals so to keep their pain away.
While the dentist must do testing to confirm their suspicions, when seen, this scenario is almost diagnostic of the patient’s tooth’s need for root canal therapy.
In cases where this home remedy works, it’s because the chilling effect of the ice lowers the pain-causing pressure inside the tooth’s nerve space by way of contracting the gases and liquids it contains.
Page references sources:
Bender IB. Pulpal Pain Diagnosis— A Review.
Germain L. Differential diagnosis of toothache pain. Part I, odontogenic etiologies.
Ingle JI, et al. Ingle’s Endodontics. Chapter: Periapical Lesions of Endodontic Origin.
Iqbal M, et al. An Investigation Into Differential Diagnosis of Pulp and Periapical Pain: A PennEndo Database Study.
Tronstad L. Clinical Endodontics. Chapter: Oral and Perioral Pain of Endodontic Interest.
All reference sources for topic Root Canals.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
The dentist filled my hurting tooth
I experienced the pain in my left side of the mouth..it was a 2nd tooth from the last that was having a space n cause pain..i went to dentist n he filled the space instead of removing but few hours later the pain started…what will be the solution?
Steven
Reply –
When a patient comes to a dentist with a tooth that aches, (hopefully) their first inclination will be to attempt to “save” the tooth if they think that makes a reasonable approach.
That often involves placing a filling in the hopes that removing the cause of the tooth’s problems (tooth decay usually) will allow it to recuperate and be OK.
What they can never know for certain is how compromised the tooth’s nerve … already was/is/has become …, and it may be that it has been traumatized enough (either by the pathology that caused the tooth’s problems and pain originally, or by the added trauma created while trying to repair the tooth) that it’s nerve tissue can’t recover, or needs more assistance in recovering.
Your solution lies in being in contact with your dentist and letting them continue to evaluate your tooth and symptoms and provide whatever type of treatment they feel is necessary.
This page explains what type of testing they may do, as well as what you may experience that can help to diagnose your condition.
As far as an outcome, one of three things will transpire.
1) Continued efforts by your dentist will assist the tooth’s recovery and it will be fine. (This might include making sure the existing filling is fine, placing a treatment/sedative filling for a while, use of medications to aid the tooth’s healing, … only your dentist can determine what’s indicated.)
2) If not, then your dentist may suggest that having root canal treatment can provide a solution to your situation. Having root canal will remove the damaged/painful/not recovering nerve tissue from your tooth. Afterward, the tooth can be rebuilt, thus returning it to full function.
3) If you decide that you don’t want to have root canal treatment, or your dentist finds a reason why they wouldn’t expect that to be successful, then the tooth should be extracted and replaced with an artificial one.
Good luck. Be in touch with your dentist’s office.
Staff Dentist
Comment –
Tooth pain.
My tooth was aching like two to five months ago .. I visited the dentist and they gave me some tablets but no treatment. But today, a national holiday, I am feeling immense pain in my teeth .what should i do ?
Hari
Reply –
You need the attention of a medical professional. A dentist would be the first choice and the one who could provide definitive treatment (root canal treatment or whatever they determine is required).
There are reasons why the same dentist you consulted with before would make a good choice. They include:
1) Although they were unable to arrive at a diagnosis the first time that they felt confident enough with to base a treatment recommendation on (which isn’t uncommon), they will have documented their findings and impressions in your chart. In cases where a tooth’s current status is still unclear, those historic notes might (but not always) help with forming a diagnosis.
2) The dentist will have the x-rays they took months ago, which can be compared to current ones taken. Having this multi-month comparison may (but not always) assist them in figuring out what your tooth’s problem is.
[Note: As your health records, you can request that the items above are sent to another dentist.]
3) Since you’ve consulted with them previously, specifically about this tooth, one would hope that your previous dentist would address your situation with some priority.
4) Your previous dentist has a copy of your medical history (which could be updated via phone) and a history of providing you with some type of medication. With those, their previous notes about your tooth, and quizzing you on the phone about your current situation, they might feel comfortable with prescribing medications via telephone before physically examining you. Doing so might give you access (like on a holiday) to needed medications sooner (pain relievers, antibiotics or whatever is indicated).
As the bottom portion of this page discusses, there’s essentially nothing that a person can do on their own to remedy their situation. And often even very little they can do to control their discomfort. You need to give this some priority and seek direct attention from a professional.
Staff Dentist
Comment –
Tooth has crown – can it need a root canal too?
I have a tooth that I had a crown put on. Maybe 8 months ago (the most). Now it has it’s own heartbeat and hurts when I chew on that side. So….is a root canal next?
SB
Reply –
Your symptoms are consistent with that of a tooth that needs root canal treatment. But of course it will take an evaluation by your dentist to know this for sure. You should definitely be in contact with them, and sooner rather than later.
If root canal is needed, that type of scenario isn’t astoundingly uncommon. We discuss dental-crown-then-root-canal situations here.
Staff Dentist
Comment –
Root canal.
ok so I have a really deep cavity in my left molar. When I was in a couple months ago my dentist told me that if it became painful then he would have to do a root canal, but I just want it extracted instead. A couple days ago I started to feel horrible pain with my tooth and I took a flosser and put it between my teeth, then I discovered that there was a small hole ( you know when you pull out your baby teeth you can stick your finger nail into the bottom of your teeth to help pull it out) and I could stick the flosser under my molar. So I plan to get my molar pulled instead, or should I get a root canal? I’m only 15!
Rhee
Reply –
If your dentist feels that they can salvage your tooth, that is typically the best plan as opposed to extraction. We have a number of sections and pages on our site that discuss various aspects of what you’ll need to think through.
Problems associated with just extracting a tooth and not replacing it.
Methods of replacing an extracted tooth if root canal treatment isn’t chosen.
Root canal vs. dental implant placement.
Staff Dentist
Comment –
Abcessed tooth/ root canal
A week ago I woke from sleep with an explosive pain in face, I looked in mirror, my right side of my face was extremely swollen, eye was swollen shut, lower part of face drooping. This was at 4am, I went to the ER thinking maybe a sinus infection, I was prescribed antibiotics by the doctor…he did no X-rays, did not look in my nose, didn’t look in my mouth. I took the antibiotics for 6 days, still having a great deal of pain, I decided to go to the dentist, after his exam it was determined I have an abcessed tooth, following day he started a root canal, he cleaned the canal, but said I have more infection that didn’t drain, he sealed the tooth and has prescribed amoxicillin, and has scheduled root canal part two in 10 days. Is this common?
VJS
Reply –
Yes, the way your dentist is treating you tooth is commonplace, and it sounds like you’re in good hands with them.
You said they sealed your tooth back up, meaning they’re trying to prevent more bacteria from entering the tooth after cleaning it somewhat.
A sealed tooth might flare up (allow pus to build up like it did before), so they’ve place you on antibiotics to make that event less likely.
They have appointed you for 10 days out, a point after you’ll have stopped taking the antibiotics. That way they’ll know if the tooth is staying quiet on its own accord, or only via the assistance of the antibiotics (a diagnostic test helping them to understand when they can complete the tooth’s treatment).
If perchance you notice problems, especially those similar to what you had before, starting to brew, let them know promptly. Most likely you’ll be fine.
Staff Dentist