Wisdom tooth infections – Pericoronitis.
1) What is pericoronitis?
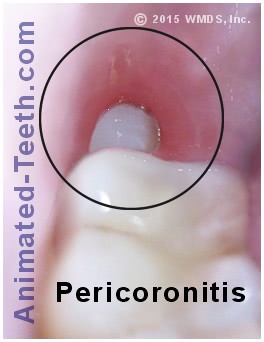
“Pericoronitis” refers to an acute bacterial infection located in the soft tissues that surround the crown portion of a partially erupted tooth. Most cases involve wisdom teeth.
- The “crown” of a tooth is its non-root portion. This is the part of a normally positioned tooth that is visible above the gum line.
- A “partially erupted tooth” is one whose crown portion has only partway penetrated through the gum tissue (see animation).
- This partially-erupted positioning may just be temporary because the tooth is still in the process of coming in.
Or it may be permanent, as in the case of a partially-erupted impacted tooth (a tooth’s whose eruption progress is blocked and therefore can proceed no further).
Where does the term “pericoronitis” come from?
- “Peri” means “around.”
- The “coron” portion of the word refers to the “crown” of the tooth.
- The suffix “itis” refers to the presence of inflammation.
Altogether, the term pericoronitis refers to the presence of inflammation in the tissues that surround a tooth due to an infection associated with its (submerged in the gums) crown portion.
2) Details about Pericoronitis. –
a) What causes it? – It’s caused by bacteria.
The underlying process/problem associated with pericoronitis is an infection, typically caused by ordinary oral bacteria (like those routinely found in the mouth).
The scenario involved is one where bacteria have colonized the space (a sac) that exists between the crown portion of the tooth and its surrounding gum tissue.
It’s the gum relationship around a partially-erupted tooth that allows pericoronitis to occur.
- The sac is formally termed a “follicular sac,” and its tissues played an important role in the formation of the wisdom tooth.
- Once the tip of the wisdom tooth has penetrated through the surface of the gums, the integrity of the sac is lost and bacteria are able to seep into it.
- Since the area within the sac is impossible to clean, a bacterial colony (dental plaque) will form within it.
The bacterial colony may have (and probably has) been present for an indefinite period of time. However, no symptoms are noticed because the person’s body defense mechanism (immune system) has been able to keep it in check.
However, if some type of event is able to tip this balance (illness, gum tissue trauma, increased numbers of bacteria or a better food supply for them), an active phase of infection (redness, tenderness, pain, swelling) can be triggered.
How often will pericoronitis form? – Transient vs. persistent episodes.
As long as a tooth remains partially erupted and is impossible to effectively clean, a person may experience repeated episodes of pericoronitis with that tooth.
- Transient – In cases where the tooth is in the process of coming in, the problem should just be a transitory one. Once the crown of the tooth fully clears the gum line, it should be possible to properly clean (brush and floss). If so, no more episodes of infection will occur.
- Persistent – In cases where the tooth is both partially erupted and impacted (meaning no further progress through the gum tissue will occur), it’s common, and even likely, that the person will experience repeated infections.
▲ Section references – Hupp, Koerner, Wray
b) Concerns with pericoronitis – The spread of infection.
A complicating factor associated with pericoronitis is that the infection that was initially just localized around the culprit tooth can then spread throughout neighboring tissues, possibly spectacularly so.
Normal conditions.
As mentioned above, since the space around a partially-erupted tooth can’t be cleansed, it always harbors a bacterial colony.
And as those bacteria create waste products, their debris simply vents off into the mouth through the same opening into the sac that the bacteria initially entered in through.
What starts as a localized infection around the tooth can spread into associated tissues.
Active phases.
As a result, the greater number of bacteria and debris (pus) now being created by the infection no longer have a way to vent off.
These items will remain locked in the area’s tissues, and cause further swelling. And if a pathway can be found, these items will force themselves into associated structures too, like a person’s face or neck.
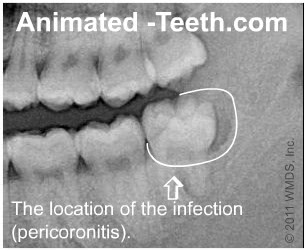
The initial formation of infection around a lower partially erupted wisdom tooth.
3) What are the signs and symptoms of having pericoronitis?
A person will characteristically notice:
- Signs of infection immediately surrounding the wisdom tooth. (Soft tissue redness, tenderness, and swelling.)
- A foul odor and/or taste coming from the infected area.
- The presence of discomfort or pain.
- Trismus. (Reduced jaw function/limited opening/muscle spasms.)
- The episode may be accompanied by fever, chills, and/or malaise.
Specific details about symptoms you may notice.
- Beyond just immediately around the tooth, with some cases, swelling associated with pericoronitis may extend into the face and neck.
- This expansion of the swelling may make it difficult for the person to open their mouth or swallow.
- The lymph nodes that service the infected region (like those under the jaw and in the neck) may become tender and enlarged.
- The amount of pain that’s experienced can be quite variable, ranging from just mild, to moderate, or even severe.
Some episodes of pericoronitis have the potential to be life-threatening.
Related to the anatomy of the region, it’s possible for an infection located in the soft tissues surrounding a lower wisdom tooth to spread rapidly and extensively into the region of the throat and neck.
If so, the extended tissues may interfere with the person’s ability to breathe and swallow, thus causing a potentially life-threatening situation. These cases may require hospitalization and possibly surgery to drain the infection.
Especially for this reason, if you notice the signs and symptoms of developing pericoronitis, you should advise your dentist sooner rather than later.
5) How is pericoronitis treated?
A dentist’s initial (in-office) treatment for pericoronitis usually includes the following steps:
The bacteria that cause pericoronitis inhabit the soft-tissue sack that surrounds the impacted tooth.
- Flushing bacteria from around the tooth.
- Establishing a path of drainage for pus.
- Providing patient instruction in how to accomplish the above two points at home.
- (Only when indicated) initiating a course of antibiotics.
- Providing pain-management instructions, possibly including prescription pain relievers.
Print out for discussion with your dentist.
We provide further details about all of these points in our discussion below.
Details about treating pericoronitis.
- Reducing the bacterial load. – As a primary objective, a dentist will remove as much of the detritus (bacteria, their waste products and associated debris) that are harbored in the under-the-gum-line space that surrounds the tooth as they can. They’ll do this by way of gently irrigating (flushing out) and/or tenderly debriding (cleaning by scraping out) the area.
- This is an important initial step. Doing so reduces the number of bacteria that are present and disrupts their living environment. And accomplishing both of these factors will ultimately help to reduce the total amount of bacterial byproducts (pus) that are produced.
- The act of gaining access to the space around the tooth when cleaning it out serves to establish a drainage pathway for pus, which in turn, helps to bring down and/or limit the amount of swelling associated with the patient’s event.
A dentist may pack gauze in the opening of the pathway they’ve created so to ensure that it stays open. (Gauze impregnated with iodoform, and antibacterial agent, is often chosen for this function.)
- In cases where a person’s symptoms are limited to localized swelling and pain, the steps above may be all that’s needed to set the stage for their recovery. If instead they also display signs of facial swelling, trismus (limited range of motion of the jaw) and/or low-grade fever, their dentist may consider prescribing a regimen of antibiotics.
FYIs about antibiotic use.
In light of current concepts governing the (over) use of antibiotics, for mild cases, the other (hands-on) steps mentioned in the list above are usually satisfactory and no course of antibiotics is prescribed.
- When not indicated at the time of your appointment, placing you on an antibiotic does little more than create a risk for your experiencing an adverse reaction to it, with your potential for any benefit being just minimal.
Of course, you will need to monitor your situation and advise your dentist if the nature of your condition changes.
- When their use is indicated, it usually takes on the order of 24 hours for oral antibiotics to begin to have an affect.
Your dentist will also provide instructions about what you should do at home.
Tooth irrigation.
In most cases, your dentist will want you to continue to irrigate (gently flush out) around your tooth three or four times a day, for the next several days.
As discussed above, doing so removes bacteria from around your tooth, disrupts their living environment and maintains a path of drainage for infection byproducts (pus). Accomplishing these factors will help to limit and ultimately resolve your condition.
Instructions.
While your dentist will tailor a set of instructions specifically for you (read on below), in short, they will include the following points …
Tooth irrigation | Rinsing around an infected wisdom tooth.
- You’ll fill a blunt-tipped syringe with irrigating solution. Saline solution (saltwater) is common.
- The tip of the syringe is placed at the junction of the tooth and surrounding gum tissue. (With loose tissue, the tip might be placed just under.)
- The contents of the syringe are expressed slowly as to gently flush out the space that exists between the tissue and tooth. (No force or pressure should be involved.)
- Spit the expressed solution out.
Specific details about the process of tooth irrigation.
- Your dentist should provide you with an “irrigating syringe.” This is a disposable blunt-needle or plastic-tipped syringe.
The idea is that its tip is placed just under the gum tissue that lays against your infected tooth. Its contents are then gently expressed, so to slowly flood and wash out the space that surrounds your tooth.
- Your dentist will provide instructions about what type of solution you should use in the syringe. Plain water, saline solution (1/2 teaspoon of table salt in 1 cup of water), or the antibacterial oral rinse chlorhexidine (via a prescription from your dentist) are all frequent recommendations.
(Note: When chlorhexidine is used, it’s effectiveness is inhibited by certain types of compounds, including some that are routinely found in toothpaste formulations. So for maximum effectiveness, be sure to read your product’s directions.)
- Your dentist may also want you to swish your mouth and the infected area with the same solution three or four times a day.
Doing so can carry off bacteria and debris, although generally less effectively than irrigating around the tooth. In cases where significant swelling or limited jaw movement are factors, they may ask you to swish until that point in time when irrigating directly around the tooth is finally possible.
An important aspect of your home care regimen is keeping in touch with your dentist. The assumption is that with each day of your continued efforts that the signs of infection associated with your tooth will gradually subside. If not, you need to let your dentist know.
And, of course, whenever possible to arrange, you’ll need to return to your dentist’s office for complete evaluation so they can determine what treatment (see possibilities below) is needed for your tooth.
COVID-19 / Treatment access considerations.
In light of the 2020 Coronavirus pandemic, some people experiencing pericoronitis may have difficulty scheduling with their dentist. In light of this complication, we will mention the following points:
- Don’t overlook the fact that even though your dentist’s office is closed, they almost certainly have a plan in effect for handling their patients’ emergencies. And this condition certainly qualifies as one.
Even in lieu of direct treatment, their coaching on how to irrigate around your tooth, or if indicated, phoning in a prescription for antibiotics to your pharmacy, may significantly reduce the level of experience you endure.
- Classically, after evaluating a patient’s situation and providing instructions, a dentist will typically give their patient a disposable irrigating syringe to take home. We’ll point out that these syringes are also available at pharmacies (either having a blunt-end needle or a plastic-nozzle design).
- There’s nothing unique to practicing dentistry that’s required to diagnose and provide the initial care and instruction needed for pericoronitis cases. Medical professionals at any emergency facility should be familiar with this condition and capable of providing these same services too.
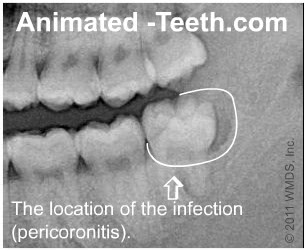
X-ray diagram showing where the infection initiates.
Definitive clinical treatment for pericoronitis.
The time period needed for this will need to be determined by the dentist treating the case but usually lies on the order of no sooner than 2 to 7 days after the patient’s initial care (establishing drainage, starting oral antibiotics (if indicated), performing rinsing and irrigation).
What long-term treatment solutions exist for pericoronitis?
- Tooth extraction is common. In cases where a decision is made to extract the wisdom tooth, the procedure should be scheduled.
- If a decision is made to retain the tooth, the dentist may feel that trimming overlying gum tissue from around it (an operculectomy) may be indicated. Or that buffing down the cusps of the opposing tooth (so they are less likely to traumatize/bite this tissue) is the solution needed.
- With other cases, a wait-and-see approach Monitoring vs Immediate removal. may make an appropriate plan.
Print out for discussion with your dentist.
4) Statistics – How frequently do people experience pericoronitis?
- Friedman’s review of published literature concluded that the incidence rate for a person experiencing pericoronitis in association with a wisdom tooth falls along the lines of 6 to 10%.
- Research frequently cites pericoronitis as being the most common reason for wisdom tooth removal. Some studies place this number as high as 40 to 59% of cases. (Faculty)
▲ Section references – Friedman, Faculty
If you experience pericoronitis, does your tooth need to be pulled?
- If it is expected that the wisdom tooth will remain impacted, and therefor at persistent risk for pericoronitis, it should be scheduled for extraction.
- If there is a possibility that the tooth will eventually erupt into normal position, a wait-and-see approach (with monitoring) is appropriate.
- For a tooth that has erupted into normal position yet excess gum tissue still places it at continued risk, performing an operculectomy may provide a solution.
Print out for discussion with your dentist.
The following discussion elaborates on the above points.
a) All teeth are just partially erupted at some point.
Just like every other tooth that comes in, even wisdom teeth that eventually fully erupt into normal and proper alignment go through a transitional period where they are only “partially erupted.”
That’s because it takes some time for a tooth to fully penetrate through the gums and achieve its final positioning. And during that time frame when the wisdom tooth is only partway through the gums, it is at risk for developing pericoronitis.
b) Partially erupted teeth are not necessarily impacted teeth.
When a dentist evaluates a patient that has pericoronitis they need to determine whether the tooth’s partially erupted status is simply a transitory phase of the normal eruption process. Or if it’s instead impacted (meaning the tooth will always remain partially erupted).
In the first case, the dentist’s approach will be to actively manage the patient’s current condition (prescribe antibiotics, irrigate the area, etc…). It’s expected then, over time as the tooth erupts more fully, that its potential for additional flareups will diminish.
In the latter case, if the impacted tooth’s positioning is not expected to resolve (come into normal position) and therefore it will always remain at risk for recurring infections, the most frequent treatment solution is extraction.
c) Operculectomy.
Some wisdom teeth that experience pericoronitis may have a relatively normal positioning in the jawbone but due to their circumstances the gum tissue that surrounds them is too “tall” or covers over them substantially.
If so, it may be possible for the dentist to resolve this issue by way of performing a minor surgical procedure termed an operculectomy. During this procedure, the unwanted gum tissue is trimmed away, with the outcome being that the tooth can now be cleansed thoroughly.
▲ Reference sources – Primary sources for this entire page: Hupp, Wray, Koerner
Page references sources:
Faculty of Dental Surgery of The Royal College of Surgeons of England. Current Clinical Practice and Parameters of Care. The Management of Patients with Third Molar (syn:Wisdom) Teeth.
Friedman J. The prophylactic extraction of third molars: a public health hazard.
Hupp J, et al. Contemporary Oral and Maxillofacial Surgery. Chapter: Principles of Management of Impacted Teeth.
Koerner KR. Manual of Minor Oral Surgery for the General Dentist. Chapter: Surgical Management of Impacted Third Molar Teeth.
Wray D, et al. Textbook of General and Oral Surgery. Chapter: Wisdom teeth.
All reference sources for topic Wisdom Teeth.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Sore gums
There are times when I can see just a part of my wisdom molar. From time to time it seems to disappear and the gums in that area get really sore. I’m afraid of having a tooth pulled.
sTs
Reply –
You’re on the right page. From your description it would seem that what you have noticed is repeated episodes of pericoronitis.
Your tooth “disappears” due to the swelling of the gum tissue around it. The pain and swelling are all symptoms of an infection surrounding your tooth because you cannot clean it properly.
You can only see a part of your tooth because it is just “partially” erupted. And it’s because your tooth has not fully penetrated your gums that you can not clean it (remove bacterial accumulation from around it) effectively.
The only question is whether the tooth will finally erupt (come through) the gums properly or not (is in it’s impacted).
If the tooth is impacted (meaning is stuck in that position), you’ll continue to experience episodes of pericoronits. (Everything we have mentioned here is explained in greater detail above on this page.)
The solution is to have the tooth taken out. The process of tooth removal really isn’t all that bad, or painful. For some people, the use of sedation medication for their procedure can place them more at ease.
Staff Dentist
Comment –
Wisdom tooth.
My wisdom tooth looks fully out. The first time i ever felt discomfort was quite young and for years ive had “appearances” where the wisdom tooth seems to disappear in the gums a little. I thought it was all over but i know somethings wrong. I’ve been trying to treat it without seeing a doctor. Now its very sore and frankly very gross (the tooths not rotten but theres quite a deep gap in my gum and i cannot clean it. It tastes bad. 🙁 ).
Ashley J.
Reply –
We agree, what you describe does seem to correlate with the common set of symptoms associated with recurring episodes of pericoronitis. You also mention that this has been going on for some years.
As you seem to already have planned, this matter does need to be pursued with your dentist because a wisdom tooth that can’t be cleansed properly potentially does place neighboring teeth at risk for damage or loss related to tooth decay and/or gum disease.
As far as the timing of your extraction, only your dentist can determine if the level of infection that currently exists is likely to complicate your procedure and therefore must be brought under control first.
Possibly your scheduling with your dentist will just happen to coincide with periods when your tooth’s condition is comparatively quiet. If so, that might speed things along. Good luck.
Staff Dentist
Comment –
Removal of impacted Wisdom tooth of person 74yrs old
4 months ago I had an upper left molar removed. When it was removed a little bit of the wisdom tooth peeked through. Now, the gum has covered a lot of the area but the wisdom tooth shows a bit more.
The dentist took x-rays and recommended removal. I know. There is always the possibility of eventual gum disease but right now after 4 months there is no pain and I try after eating anything to clean the area and never chew on that side anything hard.
Is it sensible to just wait and see in case any bacteria create future infection? Should I wait until infection develops to see him again?
Wands
Reply –
Your biggest potential for a problem with the tooth probably lies with the potential for pericoronitis (the situation discussed on this page). And then as you state, the development of complications with gum disease could be a future issue too.
It’s not exactly clear from your comment which tooth has been extracted. But if it was the one immediately in front of your wisdom tooth (the one that blocked it from coming in), now that it’s gone the wisdom tooth might erupt (thus resolving your problem configuration that allows pericoronitis to occur).
A wait-and-see approach might be considered reasonable for this type of situation but that needs to be discussed with your dentist since only they know your case and the precise configuration involved.
Staff Dentist
Comment –
Gum Flap
My wisdom tooth is coming out at the correct angle but is partially erupted, therefore leaving part of the gum hanging over the back of the tooth. I had one bad episode where the gum and my face swelled up due to infection, a few weeks ago I noticed pain in the area again so went to the dentist who cleaned out the area which then managed to resolve over the next few days, though I’m still getting some pus coming out from the gum that brings a bad taste so I went back to the dentist who gave me antibiotics, which didn’t resolve the issue so I went back again and they gave me some other ones which again, don’t seem to be resolving the problem.. I have no swelling or pain in the area just the thought of pus and the bad taste isn’t something I want to continue with.
SRC
Reply –
For the most part, oral antibiotics are taken for their systemic effect (fighting infection that has established itself within the confines of your tissues, like the swelling you experienced).
The persistent pus you notice probably comes from a focus of bacteria external to your body’s tissues, specifically in the crevice of space that exists underneath the tissue flap and around your tooth. (Some kinds of systemic antibiotics do wind up being excreted by the body into the fluids that leach into these kinds of areas, and therefore they may have a benefit, but not all are.)
Like mentioned above, with teeth in transition like yours, the person’s dentist may decide that the area needs to be “irrigated” (gently flushed out) regularly using a blunt-tipped irrigating syringe so bacteria don’t have a chance to accumulate in the space. (You’ll have to seek the advice of your dentist on this matter.)
This extra cleaning process is continued until the tooth has fully erupted and the flap of skin and its harboring/trapping debris is no longer an issue.
Staff Dentist
Comment –
Unerupted lower bottom impacted (Mesial impaction)
I have an unerupted impacted tooth (#32), it cannot be seen at all. I am 52, recently just had an infection in the area, never felt anything wrong before. The doctor think I should have both #32 and #31 extracted, and maybe an implant for #31. Is it really necessary to extract both teeth? My #31 is perfectly fine, but from x-ray, #32 is kind of leaning against it a bit. I no longer have the pain after taking some Advil, and the swelling is gone with antibiotics. With my age and history of no pain really, do I need to have both #32 and #31 taken out? Thanks!
SH
Reply –
a) The fact that you’ve experienced one infection associated with the wisdom tooth, suggests that future infections are at least possible. And the solution for one that’s impacted and completely buried by gum tissue typically would be extraction.
b) You mention that your dentist feels that if lost, #31 should be replaced. That implies that that tooth has importance (stabilizing the position of opposing teeth and possibly adjacent ones too, maintaining adequate chewing function for you, etc…). And as such, not a tooth to remove without good reason.
c) The way you phrase your comment implies that #31 is a tooth that has zero issues, and must be extracted solely to be able to remove #32.
—
1) From a technical standpoint, possibly there is something about the positioning of the impacted wisdom tooth that makes it’s extraction exceedingly difficult and by creating extra space (extracting #31), the nature of the extraction then becomes much easier.
This wouldn’t usually be the sort of treatment plan that a dentist would want to suggest. Instead, they would typically refer the extraction to a person who had a higher level of skill (an oral surgeon). One who could accomplish the extraction of #32 on its own.
If it’s already an oral surgeon who is making this recommendation to you, then one would have to assume that there is a need for this approach. Possibly the amount of jawbone removal necessary for the extraction would be excessive otherwise. We don’t know, but a explanation should be simple enough to give.
2) Probably more likely is that some current issue associated with #32, or a problem resulting from its removal, will affect/has affected #31 .
Gum disease issues (current or future) or root resorption, or decay like this page discusses, would be possibilities.
The general idea would be that the 2nd molar either has (asymptomatic) problems now, or would be expected to be left in a situation where problems would develop (gum disease, inadequate bone support) following the extraction of the wisdom tooth, thus making extraction of both and the replacement of #31 a reasonable solution.
Once again, whatever the situation, your dentist should be able to explain simply enough. Right now it seems you need more information.
Staff Dentist