Estimating the difficulty of wisdom tooth extractions.
What does a dentist look for when estimating how hard a wisdom tooth extraction will be?
Table of contents –- Why estimating extraction difficulty is important.
- Case planning – Surgical approach, procedure scheduling, patient recuperation.
- Factors that influence wisdom tooth extraction difficulty.
- The tooth’s position in the jawbone – Erupted vs. impacted. Soft-tissue vs. bony impactions.
- The tooth’s angulation (tilt/orientation).
- The tooth’s depth within the jawbone – Using the second molar as a reference.
- The tooth’s root anatomy – Curved, fused, full, or partially developed.
- What should you expect with your third molar extraction?
- Many wisdom teeth are easy to remove.
- Some will require “surgical” intervention.
- Sectioning wisdom teeth.
- Extraction difficulty will affect post-op healing and aftercare.
- Case planning – Surgical approach, procedure scheduling, patient recuperation.
- The tooth’s position in the jawbone – Erupted vs. impacted. Soft-tissue vs. bony impactions.
- The tooth’s angulation (tilt/orientation).
- The tooth’s depth within the jawbone – Using the second molar as a reference.
- The tooth’s root anatomy – Curved, fused, full, or partially developed.
- Many wisdom teeth are easy to remove.
- Some will require “surgical” intervention.
- Sectioning wisdom teeth.
- Extraction difficulty will affect post-op healing and aftercare.
How hard will your wisdom tooth extraction be?
Your dentist will have an idea, and it’s important that they do.
Long before the day of your procedure, your dentist will have made an evaluation of the level of difficulty they expect to encounter when removing your third molars.
- Their determination will influence several factors about your surgery, such as how many teeth should be removed per visit, the amount of time needed per procedure, and whether or not a recommendation for some type of sedation Conscious sedation options. might be beneficial for you.
- Your dentist’s evaluation will also determine details about how your treatment is performed.
That’s important because their choosing an appropriate surgical approach initially will help to minimize the chances for complications, both during your procedure and the healing process that follows.
- And finally, the degree of difficulty of your surgery can influence the amount of rest and recuperation sick leave you’ll require following your procedure.
How does a dentist estimate the level of challenge that a patient’s wisdom teeth pose?
Some of the best predictors of 3rd molar extraction difficulty are:
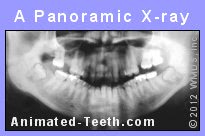
This is the most common type of x-ray used to evaluate 3rd molars.
- The position/location the tooth occupies in the jaw.
- The tooth’s angulation. (It’s orientation/tilt – Vertical, horizontal, mesio-angular, or disto-angular.)
- How deep it lies within the bone.
- The degree of formation of its roots.
- The roots’ shape and configuration. (Straight/curved, fused/separate, etc…)
Print out the list for discussion with your dentist.
We explain specific details and what you need to know about each of these factors as you read on through the remainder of this page. Or, use the links above to jump to a specific section.
FYI – All of these factors are issues that a dentist evaluates on dental x-rays (like the panoramic one shown above). So if you’re lucky enough to have already seen the pictures of your wisdom teeth, many of these points should be easy to correlate with your own situation.
Factors that influence wisdom tooth extraction difficulty.
1) The tooth’s position in the jaw.
Much of the difficulty associated with removing third molars correlates with the way they’re situated in their jawbone.
And as you might expect, generally speaking the more normal the alignment of the tooth, and the further through the gums it has pierced, the less involved its extraction and the healing process that follows, are likely to be.
Based on these parameters, dentists have developed a number of rules of thumb that they can use to estimate the degree of difficulty their patient’s 3rd molar extractions will pose.
Rules of thumb.
Erupted vs. impacted teeth.
You can expect that erupted wisdom teeth (those that have penetrated through the gums in normal fashion) will generally be easier to extract than impacted ones Classifications / Pictures (those whose eruption has stalled and are still significantly buried in gum and bone tissue).
Soft-tissue vs. bony impactions.
Soft-tissue impactions (teeth that have pierced through the jawbone substantially but are still covered by gum tissue) are typically less difficult than bony ones (teeth that are still considerably, or even completely, encased in bone).
Related graphic: Soft-tissue vs. bony impactions.
The shape of the jawbone above an impacted third molar will affect its extraction difficulty.
◄ Front of mouth. | Rear. ►
Position in the jawbone.
▲ Section references – Koerner
FYI – If you’re lucky enough to have fully erupted wisdom teeth (teeth that have come all of the way into normal position), their removal may not involve any special considerations at all and instead just be performed as routine extractions.
2) The tooth’s angulation.
The tilt of a wisdom tooth in its jawbone will affect the ease with which it can be extracted. Vertical (upright) and mesio-angular (leaning forward) impactions are typically easier to remove than disto-angular (tilted backward) or horizontal (sideways) ones.
Much of this difference is due to the extent of the surgical process required (tissue incision, bone removal). And evidence of the importance of this difference lies in the complication rates reported for each of the different classifications, with disto-angular and horizontal surgeries associated with a higher degree of swelling and reduced mouth opening postoperatively than vertical ones. (Bello)
FYI – Impacted wisdom teeth that have a pronounced tilt are more likely to need to be cut into pieces Tooth sectioning. to remove them.
This technique is used as a way of limiting the size of the wound that needs to be created to extract the tooth. That’s a positive factor for the healing process that follows. In extreme cases, sectioning might be the only way of getting a tooth out.
3) Tooth depth.
Another method of estimating the difficulty of a third molar extraction is to evaluate the tooth’s depth as compared to the adjacent 2nd molar.
The wisdom tooth’s depth is compared to the neighboring 2nd molar.
Removing this wisdom tooth can be expected to be of “moderate” difficulty.
- The 2nd molar’s root is imagined in thirds.
- The point where the dentist’s instrument (usually an elevator Extraction instruments.) will be positioned on the 3rd molar is then identified.
This point is typically where the tooth’s crown (enamel-covered portion) ends and root begins. (The white dot and arrow in our diagram lie at this level.)
- The correlation of this point and the imaginary 1/3rd divisions of the 2nd molar’s root is determined, thus indicating how hard the extraction can be expected to be.
FYI – As you’d expect, the degree of difficulty of the extraction process increases as the depth (and hence the thickness of the bone overlying the wisdom tooth) increases. A primary factor for this relationship is that the deeper a tooth lies, the harder it is to access it.
Additionally, deeply positioned teeth are more likely to be near anatomical obstacles such as nerves Possible complications. or sinuses Possible complications.. If so, the risk for surgical complications involving them elevates the complexity of the extraction process.
4) Root anatomy.
Wisdom teeth have multiple roots (lower ones typically have two, uppers usually three). And there can be quite a bit of variation in the way each is shaped.
As examples, in some cases each root will be separate and distinct. With others, one or more may have irregular contours or curvature. It’s also possible for a tooth’s roots to be fused together (either fully or partially).
As outlined below, each of these anatomical variations will affect the relative ease with which the tooth can be removed.
Rules of thumb.
In comparison to a wisdom tooth whose roots are relatively straight, distinct and separate:

Extraction difficulty is influenced by the tooth’s root form.
- Teeth whose roots are fused together (either partially or fully), especially if they have fused into a conical shape (like that of a pointed ice cream cone), are typically easier to remove.
(Erupted teeth that have conically fused roots can be astoundingly easy to extract. Upper wisdom teeth often fit this description.)
- Teeth whose roots are dilacerated (curved) or irregularly shaped can pose a greater challenge to extract. For example, those that have bulbous roots often require a substantial amount of bone trimming before the tooth can be removed.
In some cases, the direction of the root’s curvature may actually facilitate the tooth’s removal. However, in cases where that’s not the case, the root will be prone to fracture in the region of the bend.
- Teeth whose roots are just 1/3 to 2/3rds formed typically make for an easier extraction than those whose roots are fully developed. This advantage is due to both shorter root length and the fact that immature roots are generally blunt-tipped and therefore rarely fracture.
Root development is a factor that generally correlates with the age of the person. And therefore influences the ideal timing for a third molar’s removal. We discuss this and other age-related issues here: What’s the best age to have your wisdom teeth extracted?
▲ Section references – Koerner
5) Additional factors
Other factors discovered on x-rays can also signal a greater degree of difficulty for an extraction. This includes the third’s proximity (closeness) to the adjacent second molar. Or signs that suggest that the density of the jawbone is elevated.
What to expect with your third molar extraction.
More so than with any other type of tooth in the mouth, removing wisdom teeth routinely poses an assortment of challenges. And due to the range of variations possible, the way your dentist plans an extraction case will need to vary with each patient, and each tooth.
1) Some wisdom teeth are easy to remove.
You don’t have to expect the worst. In the case of a fully erupted 3rd molar (one that has come all of the way into normal position), the extraction process for it may be no more difficult than for any other molar, possibly less.
Reasons.
As compared to the molars in front of them, there’s a tendency for wisdom teeth to be slightly smaller, and more likely to have fused roots.
And especially when these factors occur in combination (a phenomenon that’s fairly commonplace with upper 3rd molars, for example), the result can be one that makes the tooth’s removal less difficult, possibly astonishingly so.
FYI – If you’re interested, this page outlines the steps that a dentist takes when performing a routine (simple) extraction How a dentist “pulls” teeth.. This is the type of process typically used to remove erupted teeth. (Compare to “surgical” extraction, discussed below.)
2) Some wisdom teeth will require “surgical” intervention.
With impacted third molars (those that still lie buried in the jaw), the dentist will, of course, need to gain access to the tooth before they can remove it. And that means they must perform a “surgical” extraction.
With this process, the surrounding gum tissue is incised and flapped back and, if needed, bone tissue is trimmed away, so the dentist can visualize and manipulate the tooth. (The link above provides more details.)
FYI – There’s no need to be overly apprehensive about the need to have a surgical extraction.
When deemed necessary, this approach typically allows the extraction process to be performed more predictably, quickly and smoothly. That’s a big positive for both your in-office procedure and the healing process that follows, thus allowing your entire experience overall to be less eventful.
Less bone removal is needed when a tooth is “sectioned” into parts.
3) Sectioning wisdom teeth.
Since each individual part is smaller than the tooth as a whole, they can be removed through a smaller access opening. This procedure is termed “sectioning” a tooth.
C) How extraction difficulty can affect patient aftercare and the post-extraction healing process.
In general, the quicker and easier it’s been for the dentist to access and remove a wisdom tooth, the less tissue trauma that’s created and the more uneventful the extraction site’s healing process should be.
As examples:
- The post-operative inconvenience and aftercare needs associated with the routine extraction of an easily accessed, fully-erupted third molar may be surprisingly minimal, to almost non-existent.
- At the other extreme, the swelling and pain resulting from a difficult impaction may require several days of recuperation.
Which scenario applies to you will simply depend on how difficult (traumatic) your extraction process has been. And thanks to the type of indicators discussed on this page, your dentist should be able to give you an idea of what to expect even before your procedure is performed.
Aftercare guidelines and directions.
For the most part, extraction aftercare is broken into two general time frames:
- The first 24 hours after your surgery. Instructions list.
- The time period 24 hours after and beyond Instructions list..
When it comes to preventing or minimizing post-operative complications, nothing is more important than following your dentist’s instructions, period. (Use the links above for more information.)
Page references sources:
Bello SA, et al. Effect of age, impaction types and operative time on inflammatory tissue reactions following lower third molar surgery.
Hupp J, et al. Contemporary Oral and Maxillofacial Surgery. Chapter: Principles of Management of Impacted Teeth.
Koerner KR. Manual of Minor Oral Surgery for the General Dentist. Chapter: Surgical Management of Impacted Third Molar Teeth.
All reference sources for topic Wisdom Teeth.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Thank you.
My son is about to have a wisdom tooth, which is at his gum line pulled. I am so nervous. This posting really helped me understand what is going on. I wish I had such a source years ago when I went through this.
Roger
Reply –
You mention that it’s your “son” – Implying a person of youngish age. Generally speaking age is a factor that favors experiencing an uneventful wisdom tooth extraction process.
You also mention that the procedure will happen fairly soon, as in possibly you are using the holiday as the recuperation period which makes a good plan just in case he needs an extended recovery period (like in the case where there is post-op swelling that needs to come down).
And you also mention that the tooth is “at his gum line.” That implies a partially erupted wisdom tooth. The kind are the most troublesome to maintain and therefore make good candidates for extraction.
Sounds like you are doing everything right. Good luck with your son’s procedure.
Staff Dentist
Comment –
Wisdom tooth near sinus.
I’m having my upper right wisdom tooth removed next week and it is partly erupted and angled towards the neighboring tooth. It has slight decay because of the angle it made it hard to brush properly. My dentist said it doesn’t seem to difficult but the oral surgeon will see on the day. The only problem is that the root is long and touches my sinus. How difficult are those type of extractions usually? I’m 31 years old by the way.
Thanks in advance.
Pete N.
Reply –
As opposed to tooth length, probably the larger factor associated with extraction ease is the configuration of the tooth’s root’s. If you’ve seen your x-ray, maybe your dentist mentioned if the roots were all separate like a tripod, or at the other extreme, fused together like a pointed ice cream cone.
With the latter, the extraction is often astoundingly simple. If the roots are separate, they simply offer more resistance form in regard to the tooth being removed.
Probably most on your dentist’s mind is the thickness of the bone in the region where your tooth approximates the sinus (it may just be paper thin).
When an extraction is a struggle, it’s possible that the tooth might push through the bone into the sinus (it’s unlikely that an oral surgeon will let this occur). Or the thin bone may fracture and create an opening into the sinus (if this occurs, an oral surgeon will know how to close the wound so healing occurs uneventfully).
It seems your dentist has your best interest in mind. They see the potential for problems, and have referred you to an oral surgeon whose knowledge and skill will make it much less likely that any problem will occur.
Staff Dentist
Comment –
Twisted roots.
Hi Today I recently seen my dentist for checking my left wisdom tooth that filling and broke for third time. The x-ray confirmed i have infection wisdom tooth and roots was twisted and needed to have extraction..my question how it caused my wisdom have twisted roots with broken tooth?
Yvonne
Reply –
It seems you are asking how the placement of a filling, or having a tooth break, or a tooth experiencing an infection, has caused the roots of that tooth to become “twisted.” Those are unrelated issues, there is no correlation between them. Instead, you have a tooth that has developed problems, that also happens to have “twisted” roots.
Staff Dentist
Comment –
Chipped upper wisdom tooth.
I’m scheduled to have an upper chipped wisdom tooth removed soon. Ive had 2 extracted in the past with sedation because they were mildly impacted.
However, the dentist didn’t refer me to an oral surgeon this time and said they could just do it in the office. Its erupted and straight, just chipped. i have some lorazepam to take for anxiety. Is it wise completing the procedure in a normal dentist office?
Thanks
S
Reply –
It’s possible that removing a upper wisdom tooth is one of the easiest extractions in the mouth.
It’s not uncommon that this tooth’s roots are fused together to form a conical shape (like a pointed ice cream cone). If so (and especially in the case where the tooth is erupted and has a normal orientation), the tooth may offer very little resistance to removal. Also, upper 3rds are often comparatively smaller teeth, and therefore have comparatively shorter roots.
While it’s impossible to state anything specific about your case, one would have to think that your dentist anticipates that some of these factors apply to your situation, and therefore they expect that your extraction process will be straightforward, and hopefully even exceedingly easy.
You state: “I have some lorazepam to take for anxiety.” You should make sure your dentist knows if you plan to take this (both quantity and when). That can be an appropriate drug to use for anxiety for an extraction procedure but they should know. Especially of concern would be how you plan to get to and return home from your dentist’s office under the influence of that medication. Best of luck with your extraction.
Staff Dentist