Signs and symptoms of failed root canal treatment –
Signs that your root canalled tooth has problems.
While the root canal therapy that’s been performed for your tooth will hopefully last you a lifetime, complications and treatment failures can and do occur. This may even take place with teeth that have a history of providing you with years, or even decades, of successful service.
This page outlines clinical signs and symptoms that are frequently associated with failed endodontic therapy. That includes both indications that you the patient may notice, and also the more subtle hints that are often only obvious to the trained eyes of a dentist.
It also provides some non-endodontic (non-root-canal-related) explanations for why you’re still experiencing discomfort with your tooth.
Page table of contents.
- Signs and symptoms of root canal treatment failure.
- Non-endodontic causes for symptoms.
- What to do?
More information about root canal failure.
As companion pages to this one, we also discuss the following associated topics:
- Why root canal treatment fails. Reasons. | Examples.
- How common is endodontic failure? Study findings.
- What further treatment or retreatment approaches Possible options. exist for failed cases?
Common Signs and symptoms of root canal failure.
A) How can you tell if your root canalled tooth has a problem?
Many of the signs and symptoms of failed or failing root canal therapy are the same ones as those that originally signaled the tooth’s need for treatment. What to look for. In brief, here are some of the things you may notice:
1) Sensitivity to pressure –
- The discomfort noticed might range from just slight tenderness to outright pain.
- It may be felt when biting/closing your teeth together, tapping on your tooth (sensitivity to percussion), or directing forces to the tooth from the side (pressing, tapping).
(When a dentist evaluates a tooth for this symptom, it’s referred to as a percussion test. How it’s done.)
The cause.
Typically this type of sensitivity is a sign of inflammation in the tissues that surround the tooth’s root.
The general scenario.
- Most cases of root canal treatment failure involve a situation where an infection has reestablished itself inside the tooth. (This link explains the types of tooth and/or treatment technical issues that frequently result in endodontic therapy failure. Our list.)
(The microorganisms involved are usually bacteria but in some cases, they may be fungi [fungus].)
- Microorganisms and infection byproducts [pus] that leak out of the tooth trigger an inflammation reaction in the tissues surrounding its root. It’s the symptoms associated with this process, in these tissues external to the tooth, that result in its sensitivity to percussion.
▲ Section references – Hargreaves, Tronstad
2) Swelling. –
Since failed endodontic cases typically do involve the presence of infection, swelling is often observed.
- The tissues affected may be limited to just those adjacent to the tooth. Or possibly even just those in the immediate area of its root tip.
At the other extreme, the swelling may be extensive and extend into the patient’s face, or even neck.
- The extent of swelling that’s present at any one point in time will simply correlate with the current level of activity of the infection, which can fluctuate (days, weeks, months).
- While not always noticeable, swollen tissues typically are tender to touch. (For this reason, palpation is an important examination method How it’s done. for a dentist to use.)

A persistent gum boil can be a sign of infection associated with failed root canal therapy.
Variants.
This page provides more detailed coverage about these lesions: What is a sinus tract? Pictures | Diagrams
3) Thermal sensitivity.
This symptom isn’t as characteristic of failed endodontic work as pain and swelling. But experiencing it is a possibility.
Since the tooth’s previous treatment removed its nerve tissue, a response to hot or cold would not be expected. But in cases where one or more of a tooth’s root canals have been overlooked and therefore not treated A common reason for failure., this type of sensitivity is possible. (Hargreaves)
▲ Section references – Hargreaves, Ingle
4) How a tooth’s symptoms may change.
The level or degree to which a person experiences symptoms can fluctuate. The time period involved might be days, weeks, or months.
- What’s noticed at any particular point in time will generally correspond with the current level of activity of the infection associated with the tooth.
- With any luck, the person’s immune system can keep the tooth’s infection in check and relatively confined within it. If so, the symptoms they notice may be quite limited.
- However, and as a worst-case scenario, teeth with failed endodontic work have the potential to flare up at any time, resulting in an acute apical abscess. What it’s like.
5) Symptom variability is common.
It must be stated that what we’ve outlined above is not all-inclusive. Your failing tooth may display additional symptoms, or possibly none at all.
Variability is commonplace, and that means that in many cases it will take your dentist’s best efforts in detection and interpretation to be able to definitively conclude that your tooth’s root canal work has failed.
B) Having symptoms doesn’t always indicate endodontic failure.
It’s possible that the symptoms you’ve noticed are not associated with your tooth’s root canal work per se. Here are some possibilities:
1) Referred pain –
The nerve that services a tooth will have the duties of servicing other teeth and structures too. And it’s possible that a dental or medical problem associated with one of them may cause sensations that just happen to feel like they’re coming from your root canalled tooth.
2) Tempromandibular joint disorder (TMJ) –
- While the actual cause of the pain is due to the TMJ condition, it may feel as though it comes from the area of a tooth, such as one that has received endodontic therapy.
- As a separate cause of pain, the excessive forces typically involved with bruxism may get directed primarily to just one or a few teeth, causing them to become sensitive (sensitivity to biting pressure would be characteristic).
When this scenario occurs in association with a tooth that has had root canal therapy, the sensitivity comes from nerve fibers within the ligament that holds the tooth in place, and therefore is not an indication of endodontic treatment failure.
3) Persistent Dentoalveolar Pain disorder (PDAP) –
PDAP disorder is a relatively new term used to label situations characterized by this set of events:
- Pain associated with a tooth signals its need for root canal therapy.
- But following its treatment, the patient continues to experience discomfort with the tooth, for months on end.
- On evaluation, nothing can be found at fault with the tooth or the endodontic treatment it has received.
PDAP cases can be especially problematic, and difficult for a person to endure. For instance, it often takes a dentist some time to finally arrive at this diagnosis. And even then, possibly only after subjecting the tooth, or even neighboring teeth, to dental procedures that have no chance of providing a solution.
And since the underlying cause of PDAP disorder is unknown, treating it is unpredictable. Complete resolution of the patient’s pain may not be possible.
We provide more information about this condition at the end of this page: Persistent dentoalveolar pain disorder. PDAP
Some signs of endodontic failure can only be detected by your dentist.
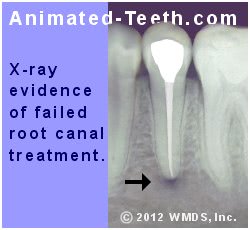
The dark spot (radiolucency) at the tip of this tooth’s root suggests that a problem exists.
C) Not all problem teeth display symptoms you can detect.
Usually what the dentist has discovered is referred to as a “radiolucency Why these form.,” like the one shown in our illustrations here.

X-ray timeline showing before and after root canal treatment and subsequent treatment failure.
The grey area of treatment success.
The point that a tooth’s work might be classified as a failure even though it remains asymptomatic brings up the issue of tooth survival vs. case success.
In endodontic terms, “survival” refers to a lack of symptoms while “success” is associated with the more rigorous standard of both an absence of symptoms and evidence of periradicular (around-the-root) tissue healing (as in no radiolucency is present).
What should you do if you suspect endodontic treatment failure?
a) If your root canalled tooth isn’t symptom-free, it should be evaluated.
For the most part, if you have a tooth that’s had root canal therapy and it continues to have or has started to show essentially any type of symptom, it should be examined by your dentist.
What’s normal.
The expectation is that following the completion of a tooth’s endodontic therapy, following an initial period of healing of the tissues that surround the root, the tooth will remain quiet and symptom-free. That’s because:
- The tooth’s nerve has been removed, so there’s no tissue inside the tooth capable of feeling sensation.
- While nerve fibers do lie in the tissues that surround the tooth’s root, successful root canal treatment resolves any issues (like infection or inflammation) that might create an irritating effect on them.
Per these two accomplishments, the tooth should remain asymptomatic (without symptoms). If it doesn’t, it should be evaluated.
b) If something seems wrong, how soon should you have your tooth checked out?
If you notice that something seems amiss with your root canalled tooth you should make contact with your dentist’s office promptly so they can determine the level of urgency associated with your case and schedule you accordingly.
Why is doing so important?
Infection typically plays a role in root canal failure, and how active it may become at any one point in time can’t be predicted. As such, teeth that have an endodontic problem have the potential to flare up at any time.
As a worst-case scenario, a long-standing low-grade infection that has only caused minor symptoms may shift into an acute phase, bringing with it intense pain and significant swelling.
Of course, just because this potential exists doesn’t mean that it will happen. But it does mean that there’s absolutely no good reason to delay in contacting your dentist’s office and seeking their attention. Once you’ve done so, they can make a determination about the urgency of your needs.
If scheduling is difficult.
In the case where you can’t be appointed to see your dentist immediately, they may feel that phoning in a prescription for antibiotics for you (either to be started immediately or to have on hand if your situation worsens (a “delayed” prescription)) can provide a means of helping to control your current symptoms and/or risk level.
However, according to current prescribing concepts, the use of an antibiotic in managing endodontic emergencies should typically play a secondary role to direct treatment. So, it is in your best interest to shuffle your schedule however is needed to accommodate whatever appointment your dentist has to offer.
c) Timing your tooth’s corrective treatment.
Once a decision has been made about the type of corrective treatment that’s required for your tooth, it should be performed within the time guidelines recommended by your dentist, for exactly the same reasons just mentioned.
Until that point in time when your tooth’s issues are finally resolved, it still remains unpredictable. And as such, it leaves you at risk for complications and/or acute flare-ups.
As a precaution, your dentist may decide to write you a prescription for antibiotics so you already have it on hand if conditions with your tooth worsen before your definitive treatment can be performed. Their decision for a need to do this will simply depend on the conditions associated with your tooth.
Note –
The remainder of this page covers the topic of Persistent Dentoalveolar Pain Disorder. This is a phantom-pain type of syndrome that only encompasses a small percentage of root canal cases where continued discomfort is experienced.
In contrast, with the vast majority of failed root canal cases, a more tangible and potentially solvable condition lies at the heart of the tooth’s symptoms. As such, you may prefer at this point to jump to associated pages that detail these kinds of problems and situations.
Associated pages menu.
Persistent Dentoalveolar Pain Disorder (PDAP).
The remainder of this page describes a syndrome where a dental patient experiences continued discomfort with their tooth that has received root canal treatment but an underlying condition associated with the tooth or its work does not seem to lie at fault.
While it’s important to include a discussion about this topic on a page that covers endodontic treatment failure, keep in mind that this syndrome only applies to a small percentage of cases.
Terminology.
The term that’s most frequently used in conjunction with this condition is “Persistent Dentoalveolar Pain Disorder” (PDAP disorder). This is, however, relatively new terminology.
(For example, Cohen’s Pathways of the pulp, likely the most used endodontic textbook in US dental schools, makes no reference to PDAP in its 2011 10th edition. In its 2016 11th edition, this term is mentioned extensively.)
▲ Section references – Hargreaves
- The signs and symptoms typically associated with PDAP cases.
- Underlying events that have been postulated to be causes of this condition.
- Treatments that may be used in the management of PDAP disorder.
- Issues and concerns that people who have this condition should be aware of.
What are the usual symptoms of Persistent Dentoalveolar Pain disorder?
The initial signs and symptoms.
The general scenario that occurs with this condition is one where:
- The patient notices discomfort with their tooth.
- Upon evaluation, their dentist determines that root canal treatment is indicated as a solution.
- Following the completion of the tooth’s treatment, its symptoms persist for months on end.
- When evaluated, no issues can be found with the quality of the tooth’s endodontic work.
That means that the initial signs and symptoms associated with what is eventually categorized as PDAP disorder start off as the same pain-related ones that typically signal a tooth’s need for root canal treatment. Example scenarios.
When is a case formally classified as persistent dentoalveolar pain disorder?
- The person’s discomfort is present on the order of at least 8 hours per day, at least 15 days per month, for at least 3 months (Warnsinck). (A criteria of 6 months is sometimes used.)
- The patient has no hesitation in identifying the tooth associated with their symptoms.
- In terms of description, the patient may state that what they feel seems to be a continuation of their original toothache. In other cases, the feeling is a new/different sensation. (Durham)
- Patients frequently describe the pain they feel as continuous, dull, and/or pressing. In some cases, the terms itching, tingling, and pricking also apply.
The pain is typically described as coming from deep within the jawbone. Its level of intensity may fluctuate throughout the day and/or as days pass. (Warnsinck)
Incidence rates.
▲ Section references – Sobieh, Durham, Warnsinck
What is the cause of PDAP disorder?
The actual underlying cause of persistent dentoalveolar pain disorder isn’t known.
Neuropathic factors.
The general consensus among experts seems to be that the pain associated with PDAP disorder has an actual neuropathic origin, as opposed to a primarily psychosocial one (Warnsinck).
As such, it would be expected that some type of lesion or disease process could be identified with cases. However, this is the conundrum that exists:
- Some type of neurological process occurs that causes the patient’s painful toothache. A condition that’s expected to be resolved by performing a deafferentation dental procedure.
(The term deafferentation means that the sensory input from the nerve is disrupted. In dentistry, this is accomplished by either removing the tooth’s nerve [via root canal treatment] or removing the entire tooth.)
- But even after the offending nerve tissue has been removed, painful sensory input still comes from the same area.
- One would anticipate that it would be a simple matter of identifying some type of condition or abnormal process in the tissues that remain. But as of yet, no type of causative pathology has been identified (Warnsick).
Psychosocial factors.
In light of the nature of the above conundrum, it’s been suggested that PDAP disorder may instead have a primarily psychosocial origin.
Some studies evaluating this issue have found no difference in these types of factors between test and control groups. However, one study did determine that PDAP disorder sufferers scored higher in the areas of depression and somatization (experiencing medical symptoms with no discernible organic cause) than the pain-free group. (Warnsinck)
▲ Section references – Warnsinck, Nixdorf
Treatment for PDAP disorder.
Treating persistent dentoalveolar pain disorder, in the sense of resolving or even just improving the patient’s discomfort level, is unpredictable. Success (total absence of pain) may not be possible.
Endodontic retreatment.
Since by definition PDAP cases involve the situation where no fault is found with the tooth’s current root canal work, conventional retreatment or other endodontic procedures (like root tip amputation) Explained. will provide no improvement.
Extraction.
Removing the tooth does not provide a solution. Since the source of the pain does not lie with the tooth itself, the discomfort will persist. (Warnsinck)
Medications.
The usual treatment approach used with PDAP cases involves a pharmacological one. Although, there is limited evidence for its effectiveness, nor is there a general consensus about which medications should be used.
- Based on the treatment of other neuropathic disorders, centrally acting oral medications (like tricyclic antidepressants and anticonvulsants [eg gabapentin]) are frequently used.
- Topical (surface) application of pain medication has been used with some success. (Capsaicin or a combination of carbamazepine, lidocaine, and ketoprofen or ketamine with gabapentin.)
Patient support.
▲ Section references – Warnsinck, Durham
Treatment outcomes.
The reality of treating PDAP patients is that success may not be possible. As an example of what might be expected, a study by Pigg followed 37 patients over a period of 7 years. It was found that:
- 13 of the participants stated that their pain status had significantly improved. 5 of these 13 reported that they were pain-free.
- 22 of the subjects (60%) considered their pain level to be unchanged or little improved.
- 2 patients felt that their situation had worsened.
Issues and considerations.
For the patient, there are several factors associated with persistent dentoalveolar pain disorder that makes experiencing it difficult.
Diagnosis.
With an incidence rate somewhere around 3% of cases or fewer, most general dentists will have little, if any, experience in diagnosing PDAP disorder.
- A worst-case scenario is one where through a failure to diagnose this condition, multiple teeth, each in turn, are suspected of being the source of the patient’s persistent pain and as a result, are subjected to root canal treatment or extraction to no avail (since neither provides a solution for this condition). This scenario is not all that uncommon.
- A complicating issue in diagnosing PDAP disorder is that a conclusion must be reached that the tooth’s current endodontic work does not lie at fault for the pain. There might be some debate as to the ability of most general dentists to arrive at this conclusion with a great degree of certainty.
Referral.
It seems easily debated that there might be benefits associated with referring the patient to a root canal specialist endodontist for evaluation fairly early in the diagnostic and/or treatment process.
- The underlying premise of PDAP disorder is that it does not stem from a deficiency with, or failure of, the tooth’s root canal work.
Due to their higher level of training and clinical experience, and usually more sophisticated equipment (like 3D x-ray imaging), it would be expected that an endodontist would be in a better position to accurately make this determination.
Either by way of identifying problems with the tooth’s current work that might be remedied. Or by knowing when to look for non-endodontic reasons to explain the tooth’s persistent pain.
- Since as a specialist their day only involves performing endodontic procedures, it would be expected that an endodontist would have much more previous experience with diagnosing and treating PDAP disorder than a general dentist.
Earlier diagnosis.
There are a number of reasons why the patient benefits if their PDAP condition is diagnosed comparatively sooner rather than later.
- Undergoing ineffectual treatment. – Typically those who suffer from PDAP disorder bounce around to a number of different practitioners (including different types of doctors) in search of resolution. Often with each one, in good faith, recommending a treatment that ultimately provides no solution at all.
- Emotional toll. – As mentioned above, experiencing this disorder can be a draining ordeal. At least with an appropriate diagnosis, some of the emotional drain associated with experiencing it might be alleviated.
- Pain centralization. – In theory, the complication of “pain centralization” may take place with longer-standing PDAP cases. (Hargreaves)
This phenomenon involves a situation where the constant pain from an area leads the central nervous system (spinal cord and brain) to become a more efficient carrier of this information.
As a result, even small inputs from the painful area are interpreted by the central nervous system as being large ones. As a worst-case scenario, treatment applied directly at the peripheral site (like numbing it up with an anesthetic) might not prevent pain from being felt.
▲ Section references – Hargreaves
Further reading about endodontic case failure:
- Why root canal treatment fails. Reasons. | Examples.
- How common is endodontic failure? Study findings.
- What further treatment or retreatment approaches Possible options. exist for failed cases?
Page references sources:
Durham J, et al. Healthcare pathway and biopsychosocial impact of persistent dentoalveolar pain disorder: a qualitative study.
Hargreaves KM, et al. Cohen’s Pathway of the pulp. Chapter: Nonsurgical retreatment.
Ingle JI, et al. Ingle’s Endodontics. Chapter: Retreatment of Non-Healing Endodontic Therapy and Management of Mishaps
Nixdorf DR, et al. Persistent Dento-Alveolar Pain Disorder (PDAP): Working towards a Better Understanding.
Pigg M, et al. Seven-year follow-up of patients diagnosed with atypical odontalgia: a prospective study.
Sobieh RM. Persistent pain following root canal therapy: A nested case series study.
Tronstad L. Clinical Endodontics. Chapter: Oral and Perioral Pain of Endodontic Interest.
Warnsinck CJ, et al. Persistent dentoalveolar pain (PDAP).
All reference sources for topic Root Canals.