Side effects caused by teeth whitening treatments.
Experiencing teeth whitening side effects is common.
Most teeth whitening methods involve the use of peroxide-based whitener. And this type of compound when used in the mouth and around teeth has the potential to cause side effects.
The precise signs and symptoms you experience (first appearance, intensity, duration, etc…) can be influenced by the kind of whitening system that’s used. For that reason, we’ve divided this page into the following sections.
Table of contents.
1) Side effects frequently associated with tray-based whitening technique.
A) Tooth sensitivity. B) Gum irritation. C) Sore throat. D) Uneven whitening.
2) Side effects frequently associated with professional (in-office) whitening treatments.
A) During in-office sessions. – 1) Tooth sensitivity. 2) Gum tissue irritation.
B) Following in-office sessions. – 1) Tooth sensitivity. 2) Tooth pain.
3) Side effects and concerns with dental work.
A) Dental composite restorations (white fillings). B) Pre-treatment issues with bonded restorations (of all types). C) Amalgam restorations (silver fillings). D) Porcelain restorations (such as bridges, crowns and veneers).
Let your dentist know that you’re having problems.
When experiencing side effects, it’s always a good idea to consult with your dentist. Transient problems are commonplace. But for peace of mind, and especially in those cases where symptoms persist or intensify, it’s best to let them pass judgment on your situation.
1) Side effects frequently associated with tray-based whitening technique.
A) Tooth sensitivity.
This is the most-reported side effect. Studies have found that roughly 1/2 to 2/3 rds of all people who bleach their teeth will notice some type of tooth sensitivity during their treatment period.
What you may notice.
What most people experience is usually just transient (one or a few days). It can be mild to moderate in intensity.
- Thermal sensitivity. – A response to hot and cold temperature variations such as those created by foods and beverages.
- Sensitivity to air. – Like when a person breathes through their mouth.
- Generalized tooth discomfort.
Who’s at risk?
There’s no way to know precisely who will encounter this problem (or to what degree). But if you notice either of the following, there’s a good chance that you will.
- Prior to starting your treatments you already notice some sensitivity to hot and cold extremes.
- You notice thermal sensitivity after getting your teeth cleaned. (For all people, it’s best to wait at least 2 weeks after a dental cleaning before starting whitening treatments.)
Solutions / Treatments.
a) Put your treatments on hold.
In a majority of cases, simply stopping all whitening activities for a few days will allow your teeth to return to normal.
Once things have settled down, consider resuming your process but using a schedule that reduces your exposure to the whitener. This could be either shortening the duration of your sessions or performing them less frequently (like every other day).
Choosing either method will mean that your overall whitening process will take a longer time frame to complete. But if that’s what it takes to keep you comfortable, then so be it.
Tip: Despite a change in your treatments, you should still be able to reach the same level of whitening results.
That’s because the lightening effect you achieve is due to your total (cumulative) exposure to the whitener. Whether this is over a relatively shorter or longer time period doesn’t matter.

10% carbamide peroxide whitener makes a good choice.
b) Use a lower concentration whitener.
You get the same results (reach the same whitening endpoint) when using a lower concentration gel, it just takes more individual treatments.
c) Use toothpaste “for sensitive teeth.”
Using “desensitizing” toothpaste can help to control side effects.
This type of product, frequently labeled as “toothpaste for sensitive teeth,” can be found on the dental aisle of just about any store that sells dental goods. The active ingredient is usually potassium nitrate or, less frequently, fluoride.

Look for toothpaste that’s for “sensitive teeth.”
Tips: The formulations of some whitening gels include potassium nitrate or fluoride. Even so, their use is seldom as effective as the extended use of desensitizing toothpaste.
- Some dentists recommend using anti-sensitivity toothpaste for 2 weeks before initiating treatments as a way of minimizing the potential for side effects.
- Another strategy is to place the toothpaste in your bleaching trays and wear them for 30 minutes a day, the entire week before initiating treatments.
d) Anti-inflammatory medicines.
The use of a non-steroidal anti-inflammatory (NSAID) medication like ibuprofen (Motrin®) can help to minimize or control bleaching-induced tooth sensitivity. (Check labeling to make sure that this type of drug is appropriate for you.)
It works by counteracting the temporary inflammation caused by the whitener as it penetrates through your tooth to its nerve tissue.
Tip: Take the medication 30 minutes or so prior to performing your treatments, that way it’s already in your bloodstream when the inflammation reaction first starts.
B) Gum irritation.
Gum tissue irritation is another frequently encountered side effect. This sensitivity can be caused either by the whitener or the bleaching trays themselves.
Causes / Solutions.
a) Use a lower concentration whitener.
Just as with tooth sensitivity, a person’s potential for experiencing gum irritation is directly related to the concentration of peroxide in the whitener they are using.
As a solution, switch to a lower concentration one (see above).
Tip: A lower risk for side effects is why our pages emphasize the use of a 10% carbamide peroxide gel with tray-based technique.
b) Halt your whitening treatments.
Noticing minor residual gum irritation after completing a whitening session can be considered normal. But this sensitivity should disappear long before initiating your next treatment.
If not, it only makes sense to stop your bleaching activities until it does. Then, once things have settled down, consider reducing your exposure to the whitener by either bleaching less frequently or for shorter periods of time (see above).
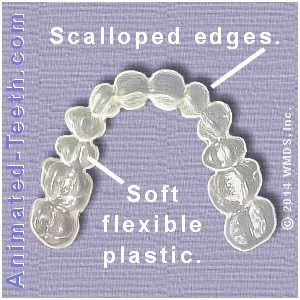
The edges of a custom tray end just short of the user’s gum line.
c) Use “custom” trays.
- These are the type you get with a dentist-dispensed system.
- Some online sources may offer dental laboratory services through which they may be obtained.
This contouring helps to minimize the contact of the whitening gel with soft tissues. And it prevents the edge of the trays from rubbing against your gums and irritating them.
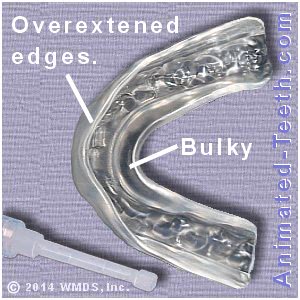
Stock trays typically cover over the user’s gums.
Stock vs. custom trays.
- If they don’t fit well, they may cause gum irritation.
- Their overextended edges can irritate gums or hold whitener against them.
Tip: Using stock trays doesn’t mean you absolutely will experience gum irritation. It just makes it more likely.
After inserting your trays, wipe away any excess gel.
d) Wipe away any excess gel.
Tip: Make sure to rinse your hands or toothbrush after doing so. Bleaching gels can damage other objects they come into contact with or irritate other body tissues.
C) Throat irritation.
It’s inevitable that during every single whitening session you’ll swallow some whitener. And as you do, it’s possible that it will irritate the tissues that line your throat.
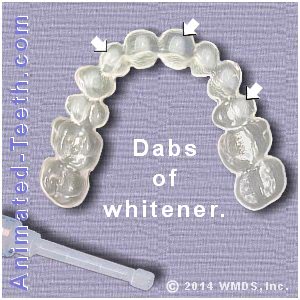
Using only dabs of whitener helps to minimize throat irritation.
Solutions / Treatments.
If the irritation persists, stop performing sessions and let things settle down. Then once they have, experiment with alternatives such as using a lower concentration whitener or performing treatments less frequently (see above).
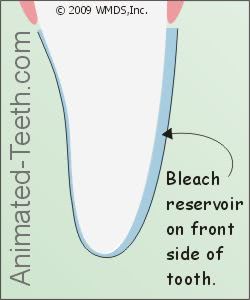
Custom trays with reservoirs helps to minimize throat irritation.
Tips:
- Dispensing only the bare minimum of whitener that’s needed can help to minimize this side effect.
- Throat irritation is more likely to occur when treatments are performed overnight as opposed to during waking hours (when you have an opportunity to spit out).
- Using custom trays designed with reservoirs (extra spaces on the front side of the teeth) help to minimize the amount of whitener that’s swallowed.
D) Uneven or spotty whitening.
A phenomenon sometimes occurs where teeth being bleached take on an uneven splotchy appearance.
This side effect is more likely to be associated with the use of whiteners that have a comparatively higher peroxide content.
Solutions / Treatment.
In most cases, the color variation will start to show during the first week of bleaching treatments and then resolve on its own (typically within a week or so as further sessions are performed).
Possible causes:
Using stock bleaching trays.
It’s possible that the use of stock bleaching trays (as opposed to custom ones, see above) is the cause of uneven whitening.
- The trays may not cover over the entire front side of each tooth, thus resulting in treated and untreated portions of the tooth.
- Any ill-fitting aspect of a stock tray may not hold the whitener in full contact with some teeth, thus leaving them under-exposed.
- (In a similar fashion, due to their standardized shape whitening strip products sometimes lack the ability to fully cover over the teeth being treated and therefore produce uneven whitening.)
Because a tooth will ultimately reach a point at which it will lighten no further, the hope is that continued treatments will allow all parts of the tooth to finally reach this end-stage and the color of all portions will match. (This may or may not be a possibility, simply depending on the nature of the tooth itself. Additionally, if the coverage of the tray, or strip, is especially deficient this may not be possible.)
Uneven whitening due to the tooth’s anatomy.
Different portions of a tooth have a different internal makeup, and this may affect the rate (evenness) with which it lightens. This effect may be especially noticeable with front teeth where:
- The thickness of the 1/2 of the tooth closest to its biting edge may be almost entirely enamel.
- In comparison, the composition of the 1/2 of the tooth closest to the gum line is one where the bulk of the tooth is composed of (comparatively dark) dentin that has an enamel covering over it.
In this situation, whatever lightening effect a single bleaching session produces will be less profound for the 1/2 of the tooth closest to the gum line because the darker appearance of the dentin underneath will still show through. The all-enamel portion of the tooth won’t have this darker layer to mask, and therefore appear whiter more rapidly.
The common (hopeful) outcome for this uneven appearance is one where the biting-edge portion of the tooth ultimately reaches a point where it whitens no further. As treatments are continued, the shade of the gum-line portion of the tooth continues to lighten and eventually (hopefully) evens things out.
How intense can whitening side effects be?
The side effects caused by a tray-whitening process may be intense enough that it has to be discontinued. But this is the exception, not the rule. In most cases what a person encounters is only minor in nature.
For most people, side effects are a non-issue.
▲ Section references – Leonard
2) Side effects frequently associated with professional (in-office) whitening treatments.
The peroxide-based tooth whiteners used with in-office treatments are formulated using the same types of compounds as tray-based at-home products. However, there are a couple of factors that make the in-office side effect experience similar but different.
- The level of peroxide content found in professional whiteners is typically much higher than with at-home products, possibly on the order of 10 times more.
- But this technique employs steps to ensure that the whitener is only applied to the patient’s teeth. It’s not in contact with soft oral tissues. None of it is swallowed.
All of these factors affect what side effects are experienced by the patient, which may appear either during or following their whitening session. Accordingly, we have divided our discussion of this topic into the following sections.
A) Side effects during in-office whitening sessions.
B) Side effects following in-office whitening sessions. – 1) Tooth sensitivity. 2) Tooth pain.
A) Side effects during treatment.
1) Tooth sensitivity.
It’s possible that you may feel a few isolated zaps or tingles during your whitening procedure. Based on the frequency or severity of what you notice, your dentist might decide that it’s best to cut your bleaching session short.
Being able to communicate with your dentist is the key here.
Set up a prearranged hand signal (or possibly your dentist will have a small bell you can signal with) so you can indicate to them that you’re experiencing sensations that need to be evaluated.
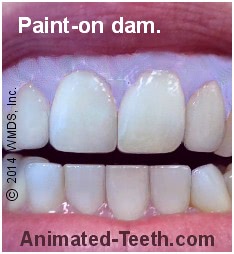
The blue (paint-on) dental dam protects the gums from irritation.
2) Gum-tissue irritation.
Why dentists don’t “numb up” whitening patients.
If the potential for experiencing pain during treatment exists, you might wonder why a dentist doesn’t just go ahead and numb up their patient’s mouth before the bleaching process is begun. The reason they don’t is that by not using an anesthetic, they make the whitening procedure safer.
- If a patient’s teeth become sensitive during their treatment process, it may be a warning sign that their session should be cut short before the nerve tissue inside them becomes seriously aggravated.
- Equally important, any pain that appears can be a warning sign that the dental dam is leaking and therefore allowing the peroxide to irritate or burn the patient’s gums, lips, or cheeks.
If the patient’s mouth had been numbed, these signals would not be available.
B) Side effects following treatments.
1) Thermal sensitivity.
After your whitening session, you may experience increased tooth sensitivity to hot and cold stimuli such as foods and beverages.
In most cases, this type of sensitivity is self-limiting and will dissipate on its own within a matter of days. However, you should always feel free to contact your dentist and report what you have noticed so they can advise you accordingly.
Professional remedies.
One remedy for thermal sensitivity is the application of fluoride to the surface of the affected teeth. And in fact, it’s common for fluoride application to be included as the last step of the in-office bleaching process.

Desensitizing toothpaste can aid in managing bleaching sensitivity..
Home remedies.
Most brands are labeled “for sensitive teeth” and contain the active ingredient potassium nitrate or else fluoride. Continued use of the product, over a period of some days and weeks, should be able to eliminate, or at least significantly reduce, the amount of sensitivity you have.
2) Tooth pain and discomfort.
You may find that you’ve experienced little if any tooth discomfort during your whitening session but then, some hours afterward, your teeth begin to hurt. This pain may range from just slight to moderate in intensity. It can come in sudden sharp episodes or else as a continuous dull ache.
This type of discomfort is usually a result of inflammation of the tooth’s nerve due to one of the following sources of irritation:
- Penetration of the peroxide bleaching agent to the tooth’s nerve.
- Dehydration of the tooth during the bleaching process.
- Exposure of the teeth to elevated temperatures for an extended period of time. (This can occur when some types of bleaching lights are used.)
As with any type of post-treatment sensitivity, you should contact your dentist so they can determine if the level of symptoms you have experienced falls within normal expectations. Doing so also gives them an opportunity to make a treatment recommendation, if needed.
Home remedies.
In most cases, this type of discomfort is self-limiting and will usually subside within just a few days.
As a treatment, your dentist may recommend the use of over-the-counter anti-inflammatory pain medications such as ibuprofen (Motrin®) or aspirin as a remedy.
- The medicine’s analgesic effect helps to control your pain.
- Its anti-inflammatory properties help to resolve your tooth’s underlying condition.
(In all cases you must read the labeling found on any drug you consider taking, so to make sure it is an appropriate medication for you.)
Preventing in-office whitening session side effects.
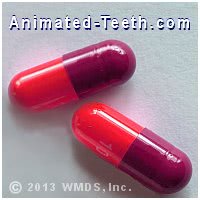
Taking anti-inflammatory medication can help with bleaching-treatment sensitivity.
Anti-inflammatory medications.
Desensitizing toothpaste.
Some dentists recommend the use of desensitizing toothpaste (discussed above) for two weeks prior to having whitening treatments as a way of minimizing your potential for experiencing complications with tooth sensitivity and discomfort.
3) Side effect issues and concerns with dental work.Will performing whitening treatments damage your dental work?
It’s easy enough to suggest that most people don’t notice any effects.
Peroxide-based teeth whiteners have been in widespread use for decades on end. (The boom in at-home whitening began in the early 1990s. And the history of dentists providing in-office treatments is much older than that.)
And during that time span, it seems reasonable to estimate that hundreds upon hundreds of millions of individual teeth and their restorations have been exposed to whiteners and the bleaching process. And from that pool, we can state that very few accounts of problems or damage caused to existing dental work have been reported. (As evidenced by a lack of cases documented in published dental literature.)
So, generally speaking, it seems that most people who have whitening treatments don’t experience any noticeable side effects or complications with their existing dental work.
That’s not to say that exposing dental work to peroxide whiteners is totally benign.
As you’ll discover as you read on, peroxide-based teeth whiteners have in fact been found to create a number of effects on dental work. However, their level of clinical importance, or when precautions should apply, is best interpreted by your dentist.
So for that reason, if you have any dental work at all that will be exposed to a whitening process, it’s always best to consult with your dentist beforehand, so they can confirm that your potential for complications seems minimal.
Harmful effects of peroxide tooth whiteners on dental restorations.
- Dental Composite restorations (white fillings).
- Pre-treatment issues with bonded restorations (of all types).
- Amalgam restorations (silver fillings).
- Porcelain restorations (such as bridges, crowns, and veneers).
A) Dental composite –
FYI: Composite resin is the type of dental restorative that’s most frequently used to create tooth-colored fillings.
Some level of deterioration probably takes place …
A number of studies have investigated the effect of peroxide-based whiteners on dental composite restorations. These evaluations have looked for changes in restoration color, surface hardness, surface roughness, staining susceptibility, restoration leakage, and bond strength.
Some studies, but not all, have reported finding measurable effects. (We discuss several of them just below.)
But in regard to their clinical significance …
▲ Section references – El-Murr
Issues of potential concern.
1) Composite hardness.
There have been conflicting reports about the effect of peroxide bleaching agents on composite resin hardness. Some researchers have documented that a decrease in both surface and/or internal microhardness does occur. Others have not identified this change.
An obvious concern related to this issue would be one of restoration strength (like its ability to withstand chewing forces). But just as important, even minor chipping at the edges of a weakened restoration could allow leakage of bacteria and contaminants, which would also ultimately lead to filling failure.
The evidence is inconclusive.
▲ Section references – El-Murr
2) Composite surface roughness.
Some studies have documented that even low peroxide (at-home use) whiteners increase the surface roughness of dental composite restorations.
Questionable clinical relevance.
One study (Wattanapayungkul) did consider the level of surface change that took place to be significant. But also determined that the degree of roughness (which was less than 0.2 microns crest-to-valley) was not great enough to aid with plaque formation and retention, and therefore was considered clinically insignificant.
▲ Section references – El-Murr, Wattanapayungkul
3) Composite restoration microleakage.
For this discussion, microleakage refers to a process where oral contaminants are able to seep past the bond that’s been created between a dental composite restoration and its neighboring tooth structure. Microleakage can result in recurrent tooth decay.
▲ Section references – El-Murr
4) Composite staining.
A study by Yu determined that dental composite restorations exposed to peroxide whiteners stained more easily than unbleached ones. Possibly this effect is related to the increase in surface roughness that takes place during the bleaching process (discussed above).
Possible solutions.
▲ Section references – Yu
5) Composite color stability.
Usually, no color change takes place …
It’s generally considered that bleaching agents won’t provide a lightening effect for white fillings (dental composite resin restorations, the most common type of white filling). (Villalta)
And as such, the usual expectation is that the patient will need to have their existing fillings replaced after their whitening treatments have been completed, so their restorations match the new shade of their smile.
If a color change occurs …
▲ Section references – Villalta, Hubbezoglu
B) Bond strength of new restorations.
This issue is of clinical importance.
It’s well documented that placing bonded restorations (white fillings, veneers, etc…) too soon after whitening treatments have been performed has the potential to significantly inhibit the strength of the bond created at the tooth-restoration interface.
This problem is thought to stem from the presence of oxygen generated during the bleaching process that still remains within the tooth’s hard tissues.
The timing that’s needed.
Studies have shown that a waiting period of at least 2 weeks is needed for the accumulated oxygen to dissipate. Then at that point, a normal-strength bond can be created.
C) Amalgam (“silver”) fillings.
Researchers investigating the effect of peroxide tooth whiteners on dental amalgam have looked for changes in restoration microhardness and surface roughness. And while some minor effects have been identified, it’s generally considered that they lie within a clinically acceptable range. (El-Murr)
▲ Section references – El-Murr
Notable issues.
1) Mercury leakage.
A laboratory study (Al-Salehi) demonstrated that exposing dental amalgam (the metal used to make “silver” dental fillings) to peroxide whiteners triggers the release of mercury and other metal ions.
- This effect can take place for up to 80 hours after exposure.
- The concentration of the whitener plays a role in the rate at which this reaction occurs. (Higher concentrations cause more of an effect.)
Studies haven’t shown that the level of mercury released exceeds World Health Organization limits (so the effect is not considered a health hazard). (El-Murr)
Treatment planning.
▲ Section references – El-Murr, Al-Salehi
2) Tarnish / Greening.
Amalgam fillings have the potential to tarnish or possibly develop a green tint when exposed to teeth whiteners. This effect is more likely to take place when higher peroxide concentrations and longer treatment times are involved.
- For this reason, silver fillings placed in teeth that hold an especially prominent position in a person’s smile are sometimes replaced with white ones before bleaching treatments are begun.
- However, the norm is that teeth that have silver fillings undergo their whitening process without significant incident.
Obviously, your dentist’s input would be a valuable asset on this issue.
D) Porcelain restorations (bridges, crowns, veneers, etc…).
Studies have shown that exposure to peroxide tooth-bleaching agents can affect the surface roughness and microhardness of some dental porcelains.
In our reading of several of these studies, it seems that this concern is most associated with “feldspathic” porcelain. (A type of ceramic that’s still in common/frequent use in dentistry but is increasingly being supplanted by more modern ones.) And the level of effect may correlate with the type of final surface treatment (glazing) the restoration has received.
A prudent approach to take when porcelain dental work is involved.
Two significant concerns that are associated with this issue are:
- If significant restoration damage or harm results (discussed below), the time and expense involved with replacing porcelain restorations can be considerable.
- It may be difficult, if possible at all, for even a dental professional to determine the nature (material, fabrication method) of some porcelain restorations.
▲ Section references – El-Murr
Issues of concern.
1) Surface roughness / Microhardness
Specifics.
In a review of this subject in 2011, El-Murr cites studies that suggest that exposing some types of porcelain-surfaced restorations to peroxide bleaching agents can result in increased surface roughness. (Specifically feldspathic porcelain restorations whose final glaze has been applied in a specific fashion. Traditionally, this type of restoration has been commonplace in dentistry.)
The problem.
The concern with this issue is that an increase in surface roughness may allow increased plaque retention (which could affect the health of the tooth’s surrounding gum tissue or possibly promote decay on the tooth or its adjacent natural teeth). Possibly the color (“whiteness”) of the porcelain may be affected too.
The review also mentions that some studies have reported changes in porcelain microhardness after being exposed to peroxide whiteners.
▲ Section references – El-Murr
Additional studies.
In investigating this issue further, we’ve found more recent studies (both by Torabi, 2014) that confirm both issues (surface roughness and microhardness changes do occur with feldspathic porcelain surfaces when exposed to peroxide whiteners).
▲ Section references – Torabi, Torabi
The needed plan when any type of porcelain restoration is involved.
In light of this information, if you have any porcelain restorations that will receive exposure to the bleaching agent, at a minimum you need to discuss this issue with your dentist beforehand. Many porcelain dental restorations are not made using feldspathic porcelain, possibly they can determine what material has been used for yours.
During that consultation, you must discuss what plan will be in place if the effects of your bleaching treatments are found to be detrimental to your restorations so there are no surprises. Replacing the restorations may be needed. In theory, it may be possible for your dentist to re-polish roughened porcelain restorations.
2) Bleaching effects on porcelain color.
In the case where it’s deemed appropriate to involve ceramic restorations in whitening activities, the person needs to understand that the color of their ceramic restorations cannot be expected to change.
This lack of effect might either be a detriment or an asset.
- If performing whitening treatments have created a color mismatch between existing porcelain restorations and natural teeth, the only solution is to replace the restorations so their color then matches.
- As a reverse approach, whitening treatments can be used to lighten natural teeth that have darkened over the years back to their lighter original shade. That way, they once again match the color of their adjacent porcelain restorations that were placed back at that time.
Porcelain veneers can be the exception.
The exception to the rule about porcelain restorations not changing color is porcelain veneers. Whitening treatments may lighten them. This page describes why this effect takes place.
Consequences.
Not understanding when your porcelain restorations will not, or possibly may, lighten can prove to be a costly affair if it leads to a need for their replacement. This issue is another prime reason why it always makes sense to mention your whitening plans to your dentist before you initiate them.
Page references sources:
Al-Salehi SK, et al. The effect of hydrogen peroxide concentration on metal ion release from dental amalgam.
El-Murr J, et al. Effects of external bleaching on restorative materials: A review.
Hubbezoglu I, et al. Effect of bleaching on color change and refractive index of dental composite resins.
Leonard R. Efficacy, Longevity, Side Effects, and Patient Perceptions of Nightguard Vital Bleaching.
Metz MJ, et al. Clinical evaluation of 15% carbamide peroxide on the surface microhardness and shear bond strength of human enamel.
Torabi K, et al. Evaluation of the effect of a home-bleaching agent on the surface characteristics of indirect esthetic restorative materials: part I–roughness.
Torabi K, et al. Evaluation of the effect of a home bleaching agent on surface characteristics of indirect esthetic restorative materials–part II microhardness.
Villalta P, et al. Effects of staining and bleaching on color change of dental composite
resins.
Wattanapayungkul P, et al. The effect of home bleaching agents on the surface roughness of tooth-colored restoratives with time.
Yu H, et al. Effects of carbamide peroxide on the staining susceptibility of tooth-colored
restorative materials.
All reference sources for topic Tray-based Teeth Whitening.
