Can a dentist pull an infected tooth? / On the same day?
Extracting infected teeth.
What’s possible?
If you have a tooth that’s been bothering you, you may be eager to have it removed ASAP. But if it’s infected, and especially if swelling is present, you may wonder if that will cause a delay in having it extracted. This page can help you understand when that might be necessary.
Table of contents –- Can a dentist pull an infected tooth?
- Sure, in a lot of cases, even on the same day.
- When the tissues around the tooth are swollen?
- Extraction may be possible, even on the same day.
- Complications and dangers associated with the presence of swelling.
- Extracting infected teeth.
- Will an antibiotic be necessary? – Before/After?
- Approaches used when delaying the extraction is necessary.
- The patient’s health status.
- Wrapping things up.
- Sure, in a lot of cases, even on the same day.
- When the tissues around the tooth are swollen?
- Extraction may be possible, even on the same day.
- Complications and dangers associated with the presence of swelling.
- Will an antibiotic be necessary? – Before/After?
- Approaches used when delaying the extraction is necessary.
Will a dentist pull an infected tooth?
Yes, dentists routinely do pull infected teeth. They do this all of the time. That’s because they know that nothing will benefit you more than just going ahead and getting rid of the source of your problem, which is your infected tooth.
Pulling the tooth is the fastest way of getting you out of pain. And once it is gone, your infection will tend to resolve more quickly and predictably.
Note: The term “infected tooth” doesn’t necessarily equate with the phrase “swollen tooth.”
A severely decayed bicuspid that shows signs of associated infection.
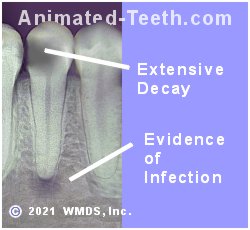
With this case, the patient was relatively asymptomatic.
Some teeth will display more active symptoms.
Sometimes an infected tooth will begin to cause some minimal level of tissue swelling and/or pain may start to become an issue.
Will a dentist pull an infected tooth when there is noticeable tissue swelling?
Yes, even when the tissues around the tooth show signs of being swollen, going ahead and removing the infected tooth promptly (same day/first office visit) is still the preferred plan.
Of course, there are always issues and factors that must be considered …
Just because tooth removal, even in the presence of swelling, makes the preferred plan for infected teeth doesn’t mean that there aren’t issues that your dentist must consider on a case-by-case basis before offering to perform your extraction procedure.
This includes factors associated with the tooth’s infection and the symptoms it has created. The patient’s health status is also of vital concern and can pose reasons to modify the treatment plan that’s utilized.
The remainder of this page discusses these types of factors. (With any of the examples given, it is assumed that the patient is a healthy individual who has an uncomplicated health history.)
What issues must be considered before extracting an infected tooth that has swelling?
Tissue swelling that has formed around an infected tooth may cause concern or present an obstacle in removing it immediately (same day). Here are some examples:
a) Swelling caused by infection may limit your dentist’s ability to access your tooth.
This reason is simple enough to understand. It may be that the amount of swelling that has formed makes it a challenge or even impossible for the dentist to have the access or visibility they feel they need to remove the tooth. This can be especially true if the level of swelling hinders the patient’s ability to open as widely as usual.
In these kinds of cases, the swelling will need to be managed before the tooth can be extracted. (Discussed below.)
b) Concerns about the effectiveness of local anesthetic.
Local anesthetics are the type of drugs dentists use to numb up teeth and oral tissues (by way of giving dental “shots”). And the chemistry of these compounds is such that they don’t work as effectively in swollen/inflamed tissues. Here’s why.

A well-defined area of swelling (pus accumulation).
If the swelling is just localized.
Localized swelling (isolated, well-defined areas of swelling) may not pose much of an obstacle to numbing your tooth and gums up for your extraction. Your dentist just needs to use a technique that numbs up the applicable nerves at a point before they enter the affected (inflamed/swollen) tissues.
▲ Section references – Fragiskos
Less localized swelling.
Tissue swelling that’s more diffuse and/or more extensive in nature may limit the dentist’s options when seeking numbing alternatives. And if so, it may be that the patient’s infection must be managed (see below) before achieving adequate anesthesia is possible and their extraction process can be performed.
Proof that it’s usually possible to numb up infected teeth even if swelling is present.
While doing research for this page, we ran across a study by Martis (1975) that evaluated 1,376 tooth extractions performed in the presence of acute infection. 327 of these teeth (almost one-fourth) even had a coexisting “fascial space abscess” (this includes the kind of tooth swelling that would be noticeable in a person’s face).
The paper’s “materials and methods” section, as more or less a side note, mentioned that “all patients were anesthetized with mandibular block for the mandibular (lower) teeth and local infiltration for the maxillary (upper) teeth.”
c) Concerns that pulling infected teeth can spread infection.
Generally, for routine, uninvolved cases involving healthy people, the belief that pulling an infected tooth will lead to the spread of infection does not pose a significant concern and therefore does not constitute a reason to not go ahead and extract the patient’s infected tooth immediately (same day/first office visit).
Historic opinion.
Most sources (textbooks, scientific papers, etc…) that discuss the issue of infected tooth extractions spreading infection explain how the consensus of the dental community has wavered over the past 100 years.
Current opinion.
Fortunately, nowadays, current practices are more likely to be guided by evidence from research studies. And they show that the removal of an infected tooth does not pose a significant risk of spreading infection.
Answers to questions about performing extractions when swelling is present –
The following sections outline different treatment protocols dentists use when extracting infected teeth and managing their accompanying infection/swelling.
1) When pulling an infected tooth, does the patient need to be placed on antibiotics first?
▲ Section references – Hupp
2) Does a person need to be placed on antibiotics after having an infected tooth pulled?
The need for a patient to be placed on antibiotics after having their tooth removed varies according to specifics about the infection/swelling that existed at the time of their extraction, and then at the completion of their procedure.
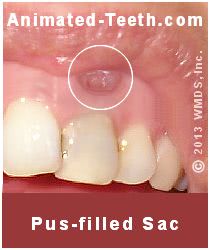
A tooth abscess (localized swelling adjacent to an infected tooth).
a) Extracting infected teeth that have minor levels of swelling.
In cases where little to no swelling is present, or else a tooth abscess has formed (an area of swelling that contains accumulated pus) but it’s well-localized and limited to an area inside the mouth and directly adjacent to the tooth (like shown in our picture), usually no postoperative antibiotic therapy is needed.
▲ Section references – Hupp
Diffuse swelling may not offer an opportunity for drainage.
b) Extracting infected teeth that have a greater level of swelling.
▲ Section references – Hupp
Research study.
The study cited above (Martis 1975) in part evaluated the implementation of this exact kind of scenario. 327 of the infected teeth removed for subjects had associated secondary “fascial space abscesses” (meaning a focus of swelling at least somewhat distant from their infected tooth).
Each patient’s extraction process included drainage of their secondary abscess. Their treatment was then followed with a course of antibiotics for at least 3 days.
▲ Section references – Martis
3) Cases where an infected tooth with swelling can’t be immediately extracted.
As mentioned above, there can be cases where the symptoms associated with a tooth’s infection make it impossible or inadvisable to go ahead and extract the tooth. If so, what can be done?

A well-defined area of swelling can frequently be drained.
i) Incision and drainage plus antibiotics.
After waiting several days (5 days is common, but depends on the dentist’s judgment), the infection has typically subsided to a level where the tooth’s extraction procedure can then be performed.
What antibiotics are used?
▲ Section references – Hupp
[Any antibiotics that are prescribed should be taken according to your dentist’s directions. If you encounter problems (including the development of a rash or itching sensation), you should report them to your dentist or physician immediately.]
Diffuse swelling may not offer an opportunity for drainage.
ii) Antibiotics alone.
▲ Section references – Fragiskos
Antibiotic therapy alone is never your dentist’s preferred choice.
It’s important to note that the use of antibiotics alone will not reliably prevent dental infections from worsening. And for that reason, it’s never your dentist’s preferred treatment approach if other options exist.
▲ Section references – Hupp, Fragiskos
d) The patient’s medical status.
Only your dentist can decide.
In all cases, whether or not to proceed with pulling your infected tooth will be a judgment call made by your dentist. There are no hard and fast rules. (Note: The common guidelines we discuss above generally apply to healthy individuals who have an uncomplicated health history.)
In addition to all of the factors we have discussed above, the patient’s current medical status is also of utmost concern. And especially when infection with swelling is involved, the patient’s ability to combat and contain that process must be weighed by the treating dentist and their treatment plan adjusted accordingly.
FAQs about pulling infected teeth.
We address the subjects of most of these Frequently Asked Questions on this page above. But for the sake of succinct clarity, here are some quick and simple answers.
Can a dentist extract an infected tooth?
Yes, doing so is possible and even common. But only if the dentist feels that they can successfully manage the challenges that the tooth’s infection poses. With severe infections, antibiotic therapy may be needed first.
Can a dentist pull an abscessed tooth?
Yes, often. Their goal will be to remove your tooth and drain the abscess.
Can a dentist pull an infected tooth without using antibiotics?
Yes, it all depends on the severity of the infection and the obstacles it poses, along with considerations for the health status of the patient. With routine cases, antibiotics are not needed.
Will a dentist pull an infected tooth the same day (first visit)?
Yes, in many cases they will because they know that’s usually what’s best for you. Doing so is the quickest way to provide pain relief and start to resolve tissue swelling.
Will a dentist pull an infected tooth if your face is swollen?
Possibly, it depends if the swelling is localized and can be effectively managed. Or diffuse and can’t be. With extensive diffuse swelling, the patient may need to be placed on a course of antibiotics first.
When should antibiotics be prescribed for an infected tooth extraction?
Only when your dentist determines that they cannot manage your condition or the extraction process without them. A common example is when extensive diffuse oral-facial swelling has occurred.
What can cause a tooth to abscess and require extraction?
Failed root canal treatment, cracks involving tooth roots, severely decayed teeth, and teeth that have advanced periodontal disease (gum disease) may abscess and require extraction.
Why won’t a dentist pull an infected tooth?
In some cases, tissue inflammation triggered by the infection may hinder numbing your tooth effectively. Additionally, associated tissue swelling can make accessing your tooth difficult or create a risk of spreading the infection.
Why can’t an infected tooth be numbed?
Inflamed tissues have an acid nature that tends to inhibit the effectiveness of local anesthetics. To counter this problem, a dentist can usually (and effectively) numb up the needed nerves at a point that lies outside of the inflamed area.
What happens if you pull a tooth that’s infected?
In terms of healing, doing so is a positive event. Pulling the tooth removes the focus of your infection and the empty socket provides a pathway for pus to drain. Your body will clear up what remains of your infection as your tooth socket heals.
How many days of antibiotics are taken for an infected tooth extraction?
When antibiotics are required (they’re very often not), using a 7 to 10-day course of antibiotics is common. The tooth is typically removed somewhere during the latter half of this regimen.
How long after starting antibiotics can an infected tooth be pulled?
Most antibiotic regimens last for 7 to 10 days. The infected tooth is typically removed somewhere during the latter half of that regimen (day 5 to 7).
Is it bad to not take antibiotics before having an infected tooth extracted?
No, in most cases antibiotics are not needed. However, this is a decision that only your dentist can make.
Do you have to finish your antibiotics before having an infected tooth pulled?
Usually not. Most dentists prefer to remove their patient’s tooth a few days before the end of their antibiotic therapy.
How many days of antibiotics are taken after an infected tooth extraction?
Starting antibiotics after your tooth extraction has been completed is not usually needed. If you started a regimen of antibiotics before your extraction, they should be taken to completion as directed.
Can an infected tooth extraction heal without antibiotics?
Yes, once the infected tooth has been removed, the extraction site will usually heal uneventfully with no antibiotic treatment needed.
Does a tooth’s infection need to be gone before your tooth extraction?
No, teeth can be pulled even though some infection is present. In fact, with necrotic teeth, the source of infection lies inside your tooth so infection will be present until your tooth has been extracted (or has had root canal treatment).
Can you still have a tooth infection after finishing your antibiotics?
In most cases, antibiotics only help your body bring infections under control, not clear them up totally. It typically takes some type of repair (tooth extraction, root canal treatment, gum surgery) to totally resolve a dental infection.
Page references sources:
Fragiskos FD. Oral Surgery (Chapter: Odontogenic Infections)
Hupp J, et al. Contemporary Oral and Maxillofacial Surgery. Chapter: Principles of Management of Impacted Teeth.
Isik BK, et al. Acutely infected teeth: to extract or not to extract?
Johri A, et al. Should teeth be extracted immediately in the presence of acute infection?
Martis CS, et al. Extractions in the presence of acute infections.
All reference sources for topic Tooth Extractions.