Cold sores & Fever blisters –
Page table of contents.
- What are cold sores?
- Causative agent – The herpes simplex virus.
- What triggers cold sore outbreaks?
- What causes sore formation? – Virion activation.
- Statistics. – Prevalence, frequency, etc…
- Primary herpetic stomatitis.
What is a cold sore?
Cold sores, also referred to as fever blisters, are a type of skin lesion caused by the herpes simplex virus that either form on a person’s lips, or else on their face in the area immediately surrounding their mouth. (The lesions display these identifying characteristics View list..)
Is there any difference between cold sores and fever blisters?
No, there’s no difference at all. These two terms refer to exactly the same type of oral lesion and can be used interchangeably.
Where do these names come from?
The derivation of these terms probably stems from the fact that a person’s outbreaks frequently correlate with periods of stress, like that caused by sicknesses such as a fever or a cold.
Additional terms.
In scientific literature, these lesions are referred to as “recurrent herpes labialis.” This term is easy to interpret when it’s broken down into its component parts:
Recurrent = Meaning something that occurs repeatedly in the same way.
Herpes = A reference to the herpesvirus, the causative agent of these lesions.
Labialis = Reference to the fact that these sores typically form on or around the lips.
What causes cold sores / fever blisters?
The causative agent of these sores (not to be confused with factors that trigger actual outbreaks View the list.) is the herpes simplex virus. But in most cases, what has caused your lesion is not the type of “herpes” that probably first comes to mind.
A little scientific background about the herpes virus.
Multiple types of herpesviruses have been identified (8 types currently) but only two of them are associated with the formation of oral-facial lesions. They are the herpes simplex virus “type 1” and “type 2.” Here are some primary differences between them.
Most cold sores are caused by Herpes Simplex – Type 1.
- Herpes simplex virus – Type 1. (HSV1)
Herpes type 1 generally only infects body tissues that lie “above the waistline,” and primarily just those that compose the orofacial area.
The tissues/regions most frequently affected are the intraoral mucosa (skin inside the mouth), the pharynx (the tissues lying just beyond the rear of the mouth), lips, eyes, and skin above the waist.
In the majority of cases, it’s HSV1 that has caused a person’s cold sore.
- Herpes simplex virus – Type 2. (HSV2)
Herpes type 2 is probably the form of the virus that first comes to a person’s mind when herpes is mentioned. However, this type usually only infects those body tissues that lie “below the waistline” (specifically the genitals or skin below the waist).
Because of that fact, HSV2 is not usually the form of the virus that causes oral lesions. However, in a small percentage of cases, it has infected the oral-facial region and therefore be the responsible agent. (Lesions caused by either type of herpes are clinically indistinguishable.)
How do you get oral herpes?
Transmission.
It’s generally considered that transmission of the herpes simplex virus occurs via direct contact with an infected individual (either their active lesion or saliva). We explain in greater detail here: HSV transmission.
The herpes simplex virus.
Making entry into your body.
▲ Section references – Agelidis, Regezi, Neville
What causes cold sore formation?
The mechanism by which the herpes virus actually causes cold sores is probably substantially different than you’d expect. Here’s how this multi-step process takes place.
1) You didn’t “just get” the herpesvirus that caused your cold sore, you already had it.
When you think of having an infection, most people would logically just assume that they were recently exposed to the germs that have caused their problem. With cold sores, however, that’s not the situation.
Cold sores are a case of virus reactivation.
- Getting a cold sore is not a sign that you’ve recently acquired a herpes simplex infection but instead, it’s a sign of the reactivation of virus particles (virions) already living inside your body How that works..
- A sore forms when herpes virions, which have been lying dormant (“asleep“) in your body, become active again (reactivate).
2) Where do the dormant virus particles come from?
The dormant virions come from an initial infection.
Primary herpetic stomatitis.
A person’s initial oral herpes infection is termed “primary herpetic stomatitis,” or alternatively “acute herpetic gingivostomatitis”.
Most primary episodes do not take the form of a cold sore. And in fact, in most cases, the person doesn’t even display any significant symptoms at all. Because of this:
- Most people don’t realize they’ve already had exposure to the herpes simplex virus.
- Or if they do, they don’t make the correlation that that episode is related to the recurrent lip and facial sores they keep experiencing.
More details about Primary herpetic stomatitis. Signs & Symptoms
The stage is now set.
Once you have experienced your initial (primary) exposure to the Herpes virus, it remains inside your body for the rest of your life.
- Most of the time, the herpes virions will lie dormant and cause no apparent effects.
- However, in response to some type of triggering event (discussed next), they can become activated. And once reactivation has begun, a cascade of events will occur that ultimately results in the formation of a cold sore breakout.
What types of events trigger cold sore/fever blister outbreaks?
A number of precipitating factors and events have been identified, however, the level of importance that any one plays for any one individual will vary.
Triggers are generally categorized as either being systemic (factors involving multiple aspects of the person’s body) or local (regional events that affect the area of lesion formation).
a) Systemic initiators –
- Emotional upset or stress.
- Physical stress and fatigue, including just being “run down.”
- Illness, fever. This can include conditions like a cold, the flu, an upper respiratory infection, or other viral infection (potentially HIV infection).
- Menstruation or pregnancy. For some women, cold sores are more frequent around the time of their monthly periods.
- Sideropenia (iron deficiency).
- Immune system weakness or deficiency. Also, treatments associated with immunosuppression (such as after an organ transplant) or chemotherapy (like that associated with treating cancer).
b) Local triggers –
- Injury (physical trauma) to the lips or surrounding skin, such as a bite, scrape, cut, or dermabrasion.
- Exposure of the lips to bright sunlight, sunburn, or an ultraviolet light source. Or extreme dryness, wind, or cold exposure that results in chapping.
- Dental treatment can act as a trigger for breakouts. This includes dental injections, periodontal procedures (gum work), and tooth extractions. Also, non-dental surgical procedures performed in the orofacial area.
▲ Section references – El Hayderi, Arduino
c) Additional factors that influence a person’s cold sore breakouts.
a) The cold-sore gene.
It’s suggested that some individuals may have a genetic susceptibility to getting cold sores.
▲ Section references – Kriesel
b) Seasonality.
We decided to look for evidence of a possible seasonal trend in cold sore/fever blister outbreaks.
Our method, and what our graph below shows, was to investigate how often people searched the Google index each month for the keywords “cold sores.” (We’re making the assumption that few people have an interest in this topic unless they’re looking for solutions for their own current/active lesions.)
As you can see, search activity for this topic seems to peak during the winter months. And that would make sense considering that it’s a time of year when people are often stressed (such as from a hectic holiday season or common cold) or exposed to harsh environmental conditions (cold, wind, dryness) that can result in lip chapping. (These events are known triggers for cold sore formation.)
Admittedly, our research method shouldn’t be interpreted as a rigorous scientific investigation.
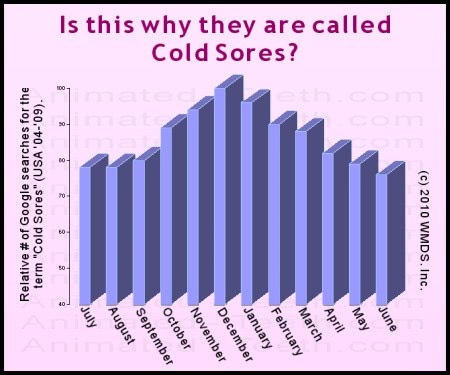
Internet search data suggests that cold sore occurrence likely peaks during the winter months.
What happens after herpes virus reactivation has been triggered?
a) Background.
Following a person’s primary oral herpes infection What to look for., some of the virus particles that were associated with that event travel along sensory nerve fibers running from the affected area to that region’s corresponding nerve ganglion.
(A ganglion serves as a hub or relay station along a nerve fiber trunk. The one usually involved with cold sores is the trigeminal ganglion.)
Once they arrive, the virions take up permanent residence. And for most of their time in the ganglion, they exist in a dormant state.
b) Viral reactivation.
The herpes virus lives in association with facial nerve fibers.
When activated, the virus forms a cold sore in the area the nerve services.
- Virus particles exit the ganglion. – The virions travel down nerve fibers that run from the ganglion to the skin tissue of the person’s perioral area (the area around the mouth).
The nerve fibers involved are those that actually service this region.
- The virions exit the nerve fibers and enter into some of the region’s skin cells Details | Pictures. Once inside, they begin to replicate (multiply in numbers).
- As the number of virions increases, the infected skin cells eventually die. This triggers an inflammation response in the surrounding tissues and culminates in ulcer formation.
With the progression of these events and the healing process that follows, the cold sore passes through its 5 stages of formation. Details | Pictures
c) Factors influencing herpes reactivation.
The conundrum.
It’s known that most of us do harbor the herpes simplex virus Statistics, yet not all people experience cold sores. Equally perplexing, of those that do, why do some people have breakouts more frequently than others?
While there’s no firm answer to these questions, herpesvirus reactivation is thought to be significantly influenced by the following component factors, each of which varies with each individual.
- The virus – This includes both the specific herpes strain as well as the number of virions residing in the ganglion.
- The triggering conditions – Factors include the relative severity of the event and the health status of the host at the time.
- Host genetics – As mentioned above, recent research suggests that a person’s genetic makeup can influence their susceptibility to the reactivation process.
▲ Section references – Kriesel
Cold sore breakouts generally correlate with periods of immune system stress.
The basic idea associated with this statement is that when normal or optimal health conditions exist, a person’s immune system is able to keep the herpes virus relatively in check. But when it’s compromised (like during sickness), the virus has an easier time overcoming body defenses, replicating and causing lesions.
- As you read through the known outbreak triggers listed above, it’s easy enough to envision how many of them correlate with periods when a person’s immune system would be under stress.
- Whereas cold sores/fever blisters are typically just a nuisance for those who are healthy, they can be a serious matter (longer-lasting, more severe) for immunocompromised individuals (people who have a chronically debilitated or compromised immune system).
Why do cold sores tend to recur in the same place?
While you may not have noticed, the details above that outline the cascade of events that take place when the herpes virus becomes reactivated also explain why cold sores tend to reoccur in the same general location each time.
The herpes virus lives in association with specific facial nerve fibers.
Once activated, the virus forms a cold sore in the area the particular nerve services.
- The herpes virus lives in association with specific nerves, and a specific nerve ganglion (the trigeminal).
- Because of that, when virus reactivation is triggered and virions begin to travel back down nerve fibers, they’re deposited in the same general skin location as with other outbreaks (see illustration).
- Since a nerve ganglion (the location where the dormant virus resides) is a type of nerve “hub,” it’s possible that on some occasions the nerve fibers traveled are different than before. If so, the cold sore that forms that time will be in a slightly different location.
How common is having the herpes simplex virus (HSV1)?
Prevalence.
It’s estimated that roughly 80% of the general population has herpes simplex virus (HSV1) antibodies in their blood. Antibodies are proof positive that a person has been exposed because our immune system only creates them in response to the physical presence of virions within our bodies.
A person typically experiences their primary HSV1 infection before the age of 20 years. And then, once your first exposure has occurred, the virus remains inside your body (active or dormant) for the rest of your life.
The good news.
Although most of us have been infected with herpes type 1, it only causes outbreaks (cold sores / fever blisters) in about one-third (20 to 40%) of the general population.
▲ Section references – Opstelten, Arduino
Locations where cold sores (fever blisters) form.
How often do cold sore breakouts occur?
- 5 to 10% of the general population experiences 6 or more outbreaks per year (Rooney), with some people having as many as 12 or more (McCarthy).
- Most people probably have somewhere between “less than 2” (Rooney) and 4 (McCarthy) per year.
- All told, somewhere between 16 to 38% of the general population suffers from these lesions.
However, the number of cold sores that a person gets typically diminishes after the age of 35 years (Opstelten). To the point whereby their senior years, only 20% of people continue to experience them. (El Hayderi)
▲ Section references – McCarthy, Rooney, Opstelten, El Hayderi
The herpes virus lives in association with specific facial nerve fibers.
Once activated, the virus forms a cold sore in the area the particular nerve services.
Primary herpetic stomatitis.
It’s your initial (primary) exposure to the herpes virus that then sets the stage where later on you (may) experience cold sores/fever blisters.
a) What are the signs and symptoms?
The signs and symptoms of a person’s initial infection of the herpes simplex virus (“primary herpetic stomatitis“) usually involve the following characteristics:
- The initial signs of the developing infection are only nonspecific in nature. They can include: fever (103 to 105 degrees F), nausea, irritability, headache, sore throat, and/or swollen neck glands.
(The incubation period following a person’s exposure can range from 2 to 20 days, with cases that produce obvious symptoms often associated with an incubation period of 3 to 9 days.)
- A day or so after the above signs have started to appear, the person’s mouth becomes painful and their gums become intensely inflamed (red, swollen, irritated).
- Usually by day three, a number of tiny, pinhead-sized (1 to 2mm) vesicles (blisters) have formed throughout the person’s oral cavity.
They may form on any oral mucosal (skin) surface, on the tongue, on the lips, or on the skin around the mouth. The number of blisters that actually form can be quite variable.
- The blisters soon rupture and tend to enlarge slightly as they transform into an ulcerated area that’s covered over by a yellowish-grey pseudomembrane (2 mm or so in size). Individual ulcerations may coalesce (merge together) into larger, irregular-shaped lesions (as large as 10 mm).
- The ulcers can be extremely painful. They often interfere with the person’s ability to eat.
- At this point, the ulcers will gradually start to heal. Mild cases may resolve in as little as 5 to 10 days. Severe cases may last up to 2 weeks.
b) Why don’t the symptoms of primary herpetic stomatitis seem familiar to you?
You were very young. – If you don’t remember having had the classic signs and symptoms mentioned above it might be because you experienced them as a small child.
- Most cases occur before the age of 7.
When affected, most individuals are between the ages of 6 months and 5 years, with most cases involving those between 2 and 3 years.
Cases before the age of 6 months are rare due to the protection of maternal antibodies.
- Previously unexposed adults can experience primary herpetic stomatitis at any age.
After age 5, a second peak of incidence tends to occur in populations involving those in their early 20’s. Cases have been reported with persons who are over 60 years of age.
Your case was very mild. – It can be that you don’t remember going through this experience because your case was subclinical.
▲ Section references – Arduino, Regezi, Neville
▲ Section references – The textbooks by Regezi and Neville were used as primary reference sources for this entire page.
Page references sources:
Agelidis AM, et al. Cell entry mechanisms of HSV: What we have learned in recent years.
Arduino PG, et al. Herpes Simplex Virus Type 1 infection: Overview on relevant clinico-pathological features.
El Hayderi L, et al. Severe herpes simplex virus type-I infections after dental procedures.
Hull CM, et al. Novel Composite Efficacy Measure To Demonstrate the Rationale and Efficacy of Combination Antiviral–Anti-Inflammatory Treatment for Recurrent Herpes Simplex Labialis.
Kriesel JD, et al. Cold sore susceptibility gene-1 genotypes affect the expression of herpes labialis in unrelated human subjects.
McCarthy JP, et al. Treatment of Herpes Labialis: Comparison of Two OTC Drugs and Untreated Controls.
Neville BW, et al. Oral and Maxillofacial Pathology. Chapter: Viral Infections.
Opstelten W, et al. Treatment and prevention of herpes labialis.
Regezi JA, et al. Oral Pathology: Clinical Pathologic Correlations. Chapter: Vesiculobullous Diseases.
Rooney JF, et al. Oral acyclovir to suppress frequently recurrent herpes labialis. A double-blind, placebo-controlled trial.
All reference sources for topic Cold Sores.
