Does a dentist really need an x-ray for every tooth extraction?
Consider this scenario …
1) A dentist has a patient in their dental chair who has a tooth that has quite a bit of mobility.
2) Related to the tooth’s looseness, it’s pretty clear to both parties that the extraction process should be exceedingly easy.
3) The patient has no interest in the dentist investigating the tooth to see if it can be salvaged.
4) They just want it pulled, and as inexpensively as possible.
So with this type of case, is an x-ray really needed for the extraction?
Our premise.
What we’ve tried to portray above is a situation that involves the simplest scenario for an extraction. Not one where explicit knowledge about the tooth’s root(s) anatomy will play a significant role in the act of removing it. (A situation where the benefit of taking an x-ray is clearly obvious.)
But instead, the case where the physics of the extraction process are so overwhelmingly in favor of the dentist that the patient could have probably even just pulled their tooth on their own, if they only had a way to numb it up.
So, even with this type of simple case, is an x-ray still always needed?
As you’ve probably already guessed, yes, in most cases you can anticipate that your dentist will still want one. The remainder of this page explains the various reasons why.
Pre and postop periapical x-rays.

FYI: What kind of x-ray is required for a tooth extraction?
- The x-ray image must show the entire tooth, and most certainly 100% of its root portion.
- The tooth’s surrounding bone tissue must be visible, so associated pathology and anatomical structures can be evaluated.
- The x-ray’s image quality must the acceptable. (Standards may vary among clinicians. | Non-digital duplicate x-rays are sometimes of poor quality.)
- The dentist must be satisfied with the image’s timeliness (date). Depending on the patient’s current circumstances, x-rays that are months old may still be considered satisfactory.
- Two or more x-rays, taken at different angles, can provide valuable additional information and may be needed.
- For routine (‘simple’) extractions – A small, individual x-ray of the tooth (a ‘PA’ x-ray) is usually all that’s needed.
If a more-encompassing image exists (like a panoramic radiograph), its use is likely suitable for single or multi-teeth ‘simple’ extraction procedures.
- For more involved extractions, including impacted teeth – A panoramic x-ray, which shows 100% of the patient’s jaws, may be required. Cone beam (3D) imaging may be required because of the added detail it can provide.
Reasons why a dentist will feel that they must take a pre-op x-ray, even for easy extractions.
1) Doing so adds another procedure they can bill for.
Just to get all cynicism out of the way first, yes, the requirement of taking a pretreatment radiograph will add to the cost of your bill for removing your tooth.
But despite the fact that your dentist may thank their lucky stars that they are in a profession where they can dictate what services are required, in reality, it’s hard to imagine that this reason alone has much to do with the way they practice dentistry.
That’s not to say that abuses with imaging don’t occur.
The type of radiograph that’s taken of your tooth can affect your bill substantially. And while it’s not expected that a patient would have the expertise to know specifically what type is indicated for their case, you can ask questions.
Generally, in increasing order of expense, here are the types of imaging used.
A periapical (PA) dental radiograph.

A periapical x-ray should show the entire tooth, including the bone around its roots.
a) Periapical x-rays (PA’s).
- By definition, this type of radiograph shows the entire tooth, root and all. (In dental usage, the word “periapical” equates with “around the root’s tip.”)
This is the least expensive type of dental x-ray (around $35). And in the vast majority of cases, this type of picture provides all of the information a dentist needs for the tooth’s extraction procedure.
b) Panoramic films.
This type of radiography shows all of a patient’s teeth and much of their associated jawbone structure. It’s cost runs on the order of $130.

A panoramic dental x-ray.
- A panoramic film excels in revealing information about the relationship between teeth (especially molars) and nearby anatomical structures (such as nerve bundles, sinuses, etc…).
- This is the standard imaging technique used in the preparation of extracting a patient’s wisdom teeth.
It’s not so common that this type of film is needed for a routine extraction (with molars being the most likely exception). Although, if it’s expected that somewhere along the line the patient will have several teeth removed, especially in different parts of the mouth, this single picture might be the one used for all of those procedures.
c) Cone Beam CT scan.
Dental Cone Beam radiography equates with taking a CAT scan of your mouth. It’s a type of 3-D imaging that can, most certainly, provide information that your dentist would otherwise have no other way to obtain. However, for most extractions, this level of detail isn’t needed.
▲ Section references – Pogrel, Vandenberghe
What usually takes place.
- A periapical film is taken first, with the expectation that it will suffice for the tooth’s extraction procedure.
- Other, more extensive/advanced forms of imaging are then only utilized if something needing greater explanation is noticed on that initial picture. (Something that your dentist should be able to explain to you easily.)
As noted above, a common exception to taking just an initial periapical film would be the situation where a panoramic x-ray [or else a full-mouth (complete) series of periapicals] is taken initially as a cost-saving measure because the need for additional extractions in the future is expected.
Bitewing x-rays.
It should be mentioned that the type of x-rays that your dentist routinely takes during checkups to look for cavities (termed bitewing radiographs) are not a satisfactory type of imaging for an extraction.
That’s because the orientation of this type of film is such that it doesn’t show the roots of teeth, which of course is the part of the tooth that’s of most concern to the dentist when removing it.
2) Taking an x-ray is the prevailing “standard of care.”
For exceedingly easy extractions, like the scenario we describe on this page, the associated “standard of care” issue probably carries as much weight about why an x-ray is taken as any other discussed on this page.
Our premise.
In this country (USA), it’s hard to imagine a dental office that doesn’t have an x-ray machine. And as we discuss below, even if exceedingly unlikely on a statistical basis, there’s always the chance that important information might be discovered by taking a pre-op radiograph. We’ll also point out that taking an x-ray prior to performing an extraction is the way your dentist was trained in dental school.
So, in the case where perchance something did go amiss with an extraction, since essentially all other dentists would have taken a radiograph first (the “standard of care”), besides experiencing the distress of causing their patient harm, a dentist could also find that they’re in serious legal trouble because they didn’t practice the same level of care that their peers routinely would have.
So, you could say that taking a pre-op x-ray of your tooth helps to ensure that your tooth’s extraction is trouble-free, both for you and your dentist.
3) There is plenty to learn from seeing an x-ray.
On this page, we’ll admit that we’ve seriously played down the value of having an x-ray for exceedingly easy extractions (like our test case described initially).
But even if a tooth’s removal isn’t expected to pose any challenge, a tooth’s pre-extraction x-ray can still provide the dentist with a lot of beneficial information. And you should want them to have it.
A severely decayed bicuspid that shows signs of associated infection.
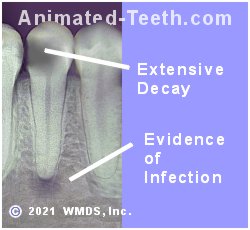
That explains why the tooth hurts. And why, if root canal therapy is not performed, it must be pulled.
a) It’s important to know why a tooth has problems.
Taking an x-ray is a valuable source of additional information for the dentist. And having it can help the dentist determine the full range of treatment options that are possible.
An example.
The preoperative x-ray shown here reveals a large carious lesion (cavity) that has formed in the tooth and shows evidence of nerve death and associated infection.
This explains why the person has had a history of experiencing throbbing pain. And if the patient is not interested in having root canal treatment performed, the x-ray confirms that having the tooth extracted is the only other available option.
b) Having more information is never a bad thing.
Even if everything about the tooth planned for extraction is as expected, an x-ray could reveal other valuable details.
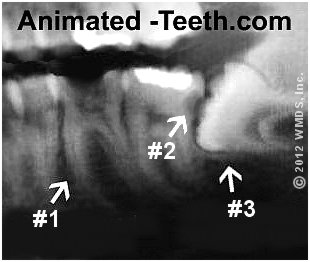
This preop x-ray has revealed additional dental problems.
An example.
Our picture here shows a portion of a panoramic dental x-ray. (By nature, its image is less sharp than periapical radiographs.)
It shows a severely decayed first molar (#1 in our picture) that the patient was already aware of. But the x-ray also shows another, totally unexpected, problem that requires immediate attention too.
The second molar has a significant amount of decay on its distal surface (backside, location #2) where debris has accumulated between it and the impacted wisdom tooth. Most likely the wisdom tooth (#3) will need to be removed before a repair can be made for the 2nd molar.
c) Documentation.
While having an x-ray of a tooth doesn’t necessarily carry more weight than information recorded in a patient’s chart as text, it certainly can be a valuable aid in documenting (often at just a glance) a tooth’s needed treatment.
- This information might be needed when planning future dental work (like that involving the extracted tooth’s space and/or its adjacent teeth). Also, an x-ray is sometimes requested by insurance companies as a part of determining what benefits will be paid by the patient’s policy.
- With impacted wisdom teeth, taking a pre-op x-ray documents the type of impaction involved, which affects billing and insurance issues.
- For more routine extractions, if the added steps of a “surgical” extraction process are performed (another factor that affects the procedure’s cost), a pre-op x-ray can help to document why these steps were needed.
4) Can’t your dentist just use your old x-rays for your extraction?
Well, in a lot of situations, previously taken x-rays may prove to be perfectly satisfactory. But only the dentist performing the procedure can decide if they are.
As an example, possibly you previously had had a full-mouth set of periapical x-rays taken during an examination appointment. Your problem tooth was identified and its treatment planned. But somehow, following through just got put on the back burner and now the tooth has started to cause problems.
If the previous x-rays give evidence of the tooth’s underlying problem, and what the dentist sees now seems to be a logical progression of that condition, they may feel that they have all of the information they require to remove the tooth without taking a new picture.
Page references sources:
Pogrel MA, et al. American Association of Oral and Maxillofacial Surgeons White Paper on Third Molar Data.
Vandenberghe B, et al. Modern dental imaging: a review of the current technology and clinical applications in dental practice. Eur. Radiol. June 2010.