Looking for information about other Dental Topics?
Full Website Index• Animated-Teeth.com •
How long do dental crowns last?
How long will your dental crown last?
While dental crowns are considered the most durable type of dental restoration, even they have a limited lifespan. Some may remain functional for decades, while others—especially crowns on front teeth, where aesthetics are paramount—may give much shorter service.
This guide explores how long a dental crown can be expected to last, based on research findings and clinical reports. It also outlines common issues that lead to replacement and how each of these tends to play a role with different types of crowns.
How long should a dental crown last?
- It can be expected that a crown should provide service for somewhere between five and fifteen years (as documented by our statistics section below).
One that has only lasted five years would most likely be a disappointment to your dentist. It’s probably their hope that any crown they make for you will last ten years or longer.
- As evidence of what’s expected, many dental insurance plans stipulate that they’ll only pay for replacements after the previous crown has been in place for 5 years.
- Depending on: 1) The amount of stress, wear, and tear the crown is exposed to (chewing and biting forces, trauma, tooth grinding) and 2) How well you keep its tooth free of dental plaque, a crown can last fairly indefinitely.
a) Statistics about crown longevity taken from dental research.
- Pjetursson (2007) performed a literature review of published research and from it estimated a survival rate of 94% for crowns at 5 years and 90% at 10 years.
- A study by Reitemeier (2013) determined that at the 8-year mark, the survival rate for porcelain-fused-to-metal (PFM) crowns lay on the order of 94% (138 teeth studied, private practice setting).
- De Backer (2007) evaluated teeth that had been crowned by student clinicians at a dental school over a 16 to 20 year period. The 18-year survival rate calculated was 75%.
- Walton (2013) reported on the long-term outcome for 2,340 crowns placed by an individual prosthodontist (a dental specialist). A survival rate of 97% was found at 10 years, 85% at 25 years.
▲ Section references – Pjetursson, Reitemeier, De Backer, Walton
b) The relative longevity of different types of dental crowns.
A literature review performed by Fernandes evaluated studies published between 1974 and 2014 pertaining to the topic of dental restoration survival rates. It concluded that:
- … gold restorations are still the “gold standard” with a 96% over 10 years survival rate, …
- … followed by porcelain-fused-to-metal crowns (PFM) (90% over 10 years), …
- … and all-ceramic crowns (75-80% over 10 years).
▲ Section references – Fernandes
(If you need some background information, here’s a link to our page that discusses types of dental crowns. Pros, cons, pictures.)
Our comments.
Due to recent advances in materials and fabrication techniques, the strength characteristics of some of the kinds of all-ceramic crowns available to dentists nowadays are substantially superior than others.
And directly to this point, the Fernandes paper reported survival rates for some modern, high-strength all-ceramic crowns (a very limited select group) to be on the same order as PFM crowns (discussed below).
The survival of the fittest seems to apply.
Once surviving past an initial period, even those kinds of all-ceramic crowns that don’t have the highest strength characteristics may ultimately provide service for as long as other types of crowns.
A study by Dhima evaluated 226 all-ceramics placed in both front and back-tooth applications. It found that:
- 6% had failed by 3.3 years (on average) after placement.
- Of those that hadn’t failed, at 5 years 95% were still in service, at 10 years 93%.
Of course, a dentist choosing to place a lower-strength type of crown in a high-stress (back tooth) application, in hopes that it would survive the first few years, thus offering evidence that the restoration should provide lasting service, would seem to be a dubious practice.
Can a failed crown just be replaced?
In most cases, the answer is most likely yes.
- If just the crown itself has experienced failure (it has cracked, broken, or no longer has acceptable esthetics, etc…), replacing it may be simple and straightforward and just involve repeating the tooth’s original crowning process. The steps. (Expect to pay a similar fee Costs for Crowns as you did the first time too.)
- If the previous crown’s failure is associated with structural damage to the tooth (it has broken, now has extensive decay, etc…), making a new one may or may not be possible. It simply depends on how much sound tooth structure remains for the dentist to work with.
Generally speaking, crowns are a method by which teeth are rebuilt. So despite however small the nub of tooth that remains, a new restoration can likely be made.
Reasons why a dental crown might fail- Signs your dentist looks for.
When your dentist examines your crown, there are a number of factors they will look for and evaluate that may indicate that your crown no longer meets its needed requirements.
In our list below, we’ve outlined the ones that we consider the most common and important, along with an indication of the type of restoration that tends to be most involved with that kind of problem. (PFM = porcelain fused to metal crown.)
Signs of crown failure your dentist will look for.
- Damage – Cracked or broken crowns | Greatest risk with all-ceramic & PFM restorations.
- Excessive wear – Hole formation | A risk with metal crowns.
- Excessive wear – Wear of opposing teeth | A risk with ceramic crowns like PFM.
- Complications with tooth decay – (All types are equally at risk.)
- Deteriorated cosmetic appearance – (Any porcelain-surfaced crown placed on a front tooth but especially PFM.)
Related page: How to tell if your crown needs replacement. Jump
Signs that a dentist associates with dental crown failure –
A) The dental crown has broken or been damaged.
If your dentist finds that your dental crown has broken, or more precisely, its porcelain component shows signs of breakage, they may conclude that your crown can no longer provide adequate service. It simply depends on the extent of the damage. (Breakage or fracture of all-metal (i.e. gold) crowns is rare.)
1) Broken porcelain crowns- What your dentist looks for.
a) With All-ceramics.
Some dental crowns have a construction where their full thickness is ceramic (e.g. all-ceramic crowns, porcelain jackets). And if this type of restoration fractures, it’s possible that the break extends through the full thickness of the crown.
If it does, the crack will compromise both the crown’s structural integrity and the seal it creates over its tooth. The only solution is to remake the restoration, no repair is possible.
Choosing the right kind of crown initially helps to avoid this problem.
The potential for failure due to breakage is a prime reason why the type of restoration you have placed on a back tooth should have a proven history of being able to withstand substantial forces. All-metal and porcelain-fused-to-metal crowns do. Some types of all-ceramics don’t and therefore will have a greater risk of failing.
High-strength dental ceramics.
Some dental ceramics have high-strength characteristics and therefore are considered appropriate for use for crowns placed on back teeth. Two of the more frequently used ones are lithium disilicate (IPS e.max®) and zirconia (BruxZir®).
▲ Section references – Fernandes
High-strength all-ceramic construction.
In applications where crown strength is of greatest concern (like with back teeth), monolithic all-ceramic crown construction probably makes the better choice. The term “monolithic” means that the restoration has been ground out of a single block of ceramic (using CAD/CAM technology).
The other method of construction for all-ceramics is one where successive layers of porcelain are fused together to create the crown.
▲ Section references – Dhima
Repair solutions for all-ceramic restorations.
- As stated above, with cracking or breakage that involves the full thickness of the ceramic, no repair is possible and replacement is required before the remainder of the restoration breaks free or decay has a chance to form underneath it.
- With small chips (cases where the seal of the crown remains intact), just rounding off or smoothing the affected area with a dental drill may suffice.
- It’s possible that moderate-sized porcelain defects can be patched, although the specific type of ceramic used to make the crown may play a role in their success.
Generally speaking, these types of repairs are just patches and likely won’t provide the same lasting service that placing a new crown would. (See our PFM section below for more details about repairing dental ceramics.)

A broken PFM dental crown.
b) With Porcelain-fused-to-metal crowns.
Background
A porcelain-fused-to-metal (PFM) crown has two components. One is a thimble of metal that covers over your tooth. The other is a layer of porcelain that’s been fused over it so to create a tooth-like appearance.
In situations where a PFM has broken, it’s typically the layer of porcelain that’s fractured off (frequently revealing the metal stub that lies underneath). It’s rare that the metal thimble itself has broken.
That means that after breaking, the seal of the crown over the tooth is still basically intact. But depending on the amount of porcelain that has come off, it’s aesthetics or function may be seriously compromised.
Repair solutions for PFM crowns.
- Minor damage might not be much of a concern and possibly remedied by just smoothing off the area using a dental drill.
- For moderate defects, placing a patch may be possible. The general difficulty is that the crown’s porcelain surface was created in a high-heat furnace but its repair must be made in the patient’s mouth.
Tooth-colored dental restorative (dental composite) can be bonded to porcelain surfaces (via acid-etching, silane coupling) but careful case selection is needed. Overall, these types of fixes are unlikely to provide the same predictable, long-term service that placing a new crown can. However, repair may offer a cost-effective solution in the interim.
Ozcam evaluated 289 repaired PFM restorations. If failure did occur, it usually took place within the first 3 months. At 3 years the survival rate for the patches was 89%. The most common reasons for repair loss were trauma, chewing failure and the fix having been performed under less-than-ideal conditions (the tooth couldn’t be kept saliva-free during its procedure).
- In cases where major damage has occurred (a large portion of the restoration is involved), a new crown will simply need to be made.
How frequently is this issue a problem?
a) A study by Behr investigated the subject of PFM crown veneer chipping. It evaluated 997 restorations that had been placed on both front and back teeth.
- Porcelain loss was only experienced by 1.7% of all of the crowns over a 10-year period.
- PFM crowns on posterior teeth (molars and premolars) fared the worst with an incidence rate of 2.7% chipping at 10 years.
Overall the findings of this study demonstrate that PFM crowns typically provide lasting service, even when placed on teeth that are regularly exposed to comparatively heavy chewing forces.
b) Reitemeier reported higher numbers. This paper determined that at 10 years the incident rate of ceramic defect lay on the order of 11%. However, it was specifically stated that the majority of events were either not treated or just smoothed and/or polished. Only 10% of the failures (and therefore only about 1% of all crowns studied) required repair or crown removal.
▲ Section references – Behr, Reitemeier
2) Crown damage as a consequence of having root canal treatment- What your dentist must evaluate.
A complication that may arise with crowned teeth is the later need for root canal treatment. The following pages explain why:
If root canal therapy is needed, the first step of this procedure involves creating an “access cavity.” This is the opening through which the dentist accesses the interior of the tooth and performs their work.
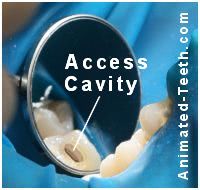
This access cavity for root canal treatment has been made through the tooth’s dental crown.
If the crown can’t be removed first, the hole will need to be made right through it. And doing so compromises the restoration’s seal over the tooth (even placing a filling in the opening can’t predictably reestablish it).
Repair solutions.
Ideal treatment involves replacing the crown after the root canal therapy has been completed. We discuss this topic and explain possible alternatives and outcomes on this page: Does a crown need to be replaced after root canal treatment? Deciding factors.
B) Crowns that show excessive wear.
Signs your dentist looks for.
Background – The ideal crown.
Dental crowns aren’t necessarily more wear-resistant than your own natural teeth, nor is it in your best interest that one should be.
The ideal dental crown would be one made out of a material that has the same wear characteristics as tooth enamel. This way neither the crown nor your natural teeth would wear the other excessively. (FYI: Gold crowns Description. and some types of all-ceramic Description. ones come closest in this regard.)

This gold crown has a hole in it.
1) Perforations (crowns with holes).
Repair solution – Since the hole compromises the seal of the crown, a new one should be made before that point in time when dental plaque has had a chance to seep under and start a cavity.
2) Worn opposing teeth.
In some cases, the problem is not that the crown has worn but instead that it has caused excessive wear of the teeth it opposes.
Repair solution – Making a new crown for the tooth out of a material that is less abrasive to tooth enamel (gold, some kinds of dental ceramics) can slow the wear rate.
Tooth decay can extend underneath the crown.
C) Recurrent tooth decay.
Signs your dentist looks for.
Dentists use the term “recurrent decay” to refer to this scenario, meaning the formation of a new cavity on a tooth that has already had a restoration placed on it.
There are two main difficulties associated with decay forming in this location.
- It’s difficult for the dentist to know the full extent of the cavity. Decay that has spread underneath the crown (see illustration) is both hard to evaluate, access and know for certain that it’s been totally removed.
- A basic tenant of crown placement is that its edges lie on sound tooth structure (this creates the most predictable, lasting seal over the tooth). Placing a filling right at the edge of a crown breaks this rule.
Repair solutions.
That’s not to say that dentists never solve this problem by just going ahead and placing a filling. But doing so is patchwork dentistry.
The textbook solution is to remove the existing restoration, remove the decay and then make a new crown for the tooth.
How frequently is this issue a problem?
The study by Behr cited above also investigated the decay rate of teeth that had received crowns.
- At 5 years, 1.3% of the crowned teeth were found to have developed a cavity.
- At 10 years, 2.8% had.
Overall this study suggests that the formation of recurrent decay is a present but relatively minor complication. The tooth’s risk increases over time.
D) The cosmetic appearance of the crown has become objectionable.
Signs your dentist looks for.
1) The crown’s edge has become visible and it has a grey appearance.
Background.
Over time, the gum line of a tooth may recede. This is especially likely in those cases where a person has been lax in their brushing and flossing habits.
If enough recession takes place, the edge of a crown (which was originally tucked out of sight just below the gum line) will become visible.
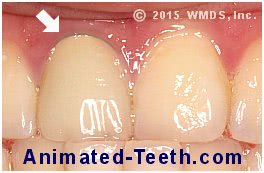
A hint of the metal edge of this PFM crown has started to show.
a) The problem with PFM’s.
And if enough gum recession occurs, this dark edge will become visible, thus spoiling the appearance of the crown.
b) All-ceramic crowns.
Because they don’t have a metal component, all-ceramic restorations don’t suffer from the grey-line problem.
However, gum recession can expose that portion of the tooth (usually the root) that lies beyond the edge of the crown. And this part usually appears darker, or at least in some way different in color from the crown itself, thus spoiling the overall appearance of the tooth.
Repair solutions.
- A dentist may make an attempt to cover over the discoloration with dental bonding (a white filling). However, even if this gives an acceptable outcome initially (which is not always the case), it’s never a long-term solution.
- The only lasting repair is to replace the crown with a new one. One that extends towards the gum line further so as to cover the now-revealed portion of the tooth.
How often does the dark-line problem occur?
We don’t have a precise estimate of how often the PFM/dark-edge issue is problematic enough that making a new crown is needed.
We did find a study (Walton) that stated that out of 2211 PFM’s evaluated over a 25-year period, 1% of them needed to be replaced due to “unacceptable esthetics,” on average after 14 years of service.
When considering that number, the following should be kept in mind:
- The restorations evaluated were all placed by a prosthodontist (crown specialist), who would be considered an expert at minimizing the potential for this complication.
- Some of the failures reported would be related to other cosmetic deficiencies too, not just the visibility of a dark line.
With both caveats considered, it seems likely that this is just an “issue” rather than an inevitable significant problem with PFM’s.
▲ Section references – Walton
2) The color of the dental crown no longer matches its neighboring teeth.
Background.

The natural teeth on each side of this crown have darkened.
Repair solutions.
- One is to replace the offending crown with a new one that more closely matches the current color of the neighboring teeth.
- Another is to use teeth-whitening treatments Technique explained. in an attempt to return the neighboring teeth back to the color they were when the dental crown was originally placed.
For more information, we suggest reading this page: What to do if the color of your crown doesn’t match. Jump
Some things to realize.
a) Prevention is always the best approach.
You’ve just learned that in most cases having a “permanent” crown placed doesn’t mean that it’s going to last forever. And that means to whatever extent is possible, one of your dental goals should be to avoid winding up in a position where getting one is needed.
Toward achieving this goal, we offer our page: Precautions to take that can help you to prevent needing to get teeth capped. Things to do.
b) Many crowns fail for preventable reasons.
The statistics above reflect the outcomes that people usually experience with their crowns. But in comparison, we couldn’t help but notice the findings of a 50-year study about restoration longevity conducted by Olley.
As the criteria for the study’s subjects:
- All were patients of a single “experienced operator.” (Implying a dentist with good clinical judgment and skills.)
- Who had been followed annually with clinical and x-ray examinations. (Had regular checkups, although just yearly.)
- And followed strict preventive practices and had excellent oral hygiene. (One would have to assume that effective brushing and flossing on a daily basis would play a big role in achieving this.)
Admittedly, with these restrictions and the long time span involved, the study only included the evaluation of a relatively small number of restorations (about 200 crowns).
The study’s findings.
- The mean survival for metal-ceramic crowns (PFM’s) was over 47 years.
- Gold (posterior tooth) and all-ceramic (anterior tooth) crowns had 100% survival at 50 years.
Our comments.
There’s essentially nothing reported by this study that surprises us. It simply documents that well designed and crafted crowns, if their tooth is kept plaque-free, can last essentially indefinitely.
We can see how some of the cosmetic issues discussed above might arise. (Adjacent teeth do tend to darken and gum lines do tend to recede with age.) And therefore placing a new crown may be warranted if the problem can’t otherwise be managed.
Page references sources:
Behr M, et al. The clinical performance of porcelain-fused-to-metal precious alloy single crowns: chipping, recurrent caries, periodontitis, and loss of retention.
De Backer H, et al. Long-term survival of complete crowns, fixed dental prostheses, and cantilever fixed dental prostheses with posts and cores on root canal-treated teeth.
Dhima M, et al. Practice-based clinical evaluation of ceramic single crowns after at least five years.
Fernandes NA, et al. The longevity of restorations – a literature review.
Olley RC, et al. An up to 50-year follow-up of crown and veneer survival in a dental practice.
Ozcan M, et al. Clinical study on the reasons for and location of failures of metal-ceramic restorations and survival of repairs.
Pjetursson BE, et al. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs).
Reitemeier B, et al. A prospective 10-year study of metal ceramic single crowns and fixed dental prosthesis retainers in private practice settings.
Walton TR. The up to 25-year survival and clinical performance of 2,340 high gold-based metal-ceramic single crowns.
All reference sources for topic Dental Crowns.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Lower crown with a small spot worn through the gold crown.
What are my options? I have no pain and the crown is 40+ Year’s old.
Gail
Reply –
From the standpoint of crown strength or appearance, the perforation is probably a non-issue. However, what your crown no longer does is predictably provide a seal over the tooth.
In theory, bacteria could leak through the opening and cause decay. And for that reason making a new crown, in theory, offers the best solution.
From a practical standpoint, your dentist may decide that they can adequately monitor the perforation for developing problems without any immediate treatment.
Or they may feel that placing a filling in the opening seals the tooth predictably enough.
Staff Dentist
Comment –
Crown keeps coming off.
Previously root canal tooth with crown. Crown has come off twice! Swallowed the most recent one! I have decided to get it extracted and get an implant.
MG
Reply –
For anyone else reading, it wouldn’t be customary to extract a tooth only because it’s crown keeps coming off.
In MG’s case, there must be shortcomings associated with the tooth that prevents their dentist from having the option of being able to improve the retention form (shape) of the tooth and making a new crown.For anyone else reading, it wouldn’t be customary to extract a tooth only because it’s crown keeps coming off.
Staff Dentist
Comment –
Why replace crown?
40 years ago I broke my front tooth. Recently, the crown and post fell out, because of decay. The decay was repaired and I assume a filling was done on the real tooth under the crown. I’ve had different dentists suggest implants and bridges. My question is,even tho there is a filling there now, why cant a core building happen to build up the tooth to what it was before and then put back the crown and post, or even a new crown and post?
Curtis C
Reply –
We don’t follow your description entirely but think your situation is:
1) You had a post & core and crown placed 40 years ago.
2) Recently, related to the development of decay, that restoration work fell out.
3) A dentist removed the decay, and then recemented the original post and core.
4) But after that, that dentist stated to you that they thought extraction of the tooth and replacement of the tooth via a bridge or implant was indicated. Other dentists who have seen your tooth have stated the same thing.
One would have to assume that possibly:
1) The decay involved a substantial aspect of the tooth that lies below the gum line. This page explains why subgingival (below the gum line) issues are a problem. (The page is about broken teeth, but the same challenges would apply with tooth structure lost to decay.)
With a front tooth (and the cosmetics involved), changing the level of the gum line might not give an acceptable result.
If the gum line level was changed, possibly due to the extent of the decay the amount of root length still encased in bone would be too short to provide suitable tooth stability.
2) The dentist may feel that what’s now left of the tooth offers big challenges in being able to adequately (securely, predictably) anchor a post and core to it.
—
Whatever decay existed had to lie beyond the edge of the existing crown (decay can’t penetrate through a crown). So now that the decay has been removed, it’s edges no longer fully lie on sound tooth structure (at least one part would rest on an area of filling).
Structurally that’s a weak configuration. And it also means that the existing crown no longer creates a predictable seal over your tooth (the weak link being the fit in the area of the filling).
So even if somehow your tooth is restored with a post & core and crown, all of the components will need to be new ones to do the job right.
Staff Dentist
Comment –
Crown replaced.
Had new crown placed on last lower molar that was cracking and had old fillings, but NO pain.
Dentist placed new crown on tooth, which did not need a root canal done. Less than six months later the new crown badly cracked, but there was still NO pain. Dentist removed cracked crown and replaced it with a new one. NOW I am having heat/cold sensitivity and pain while chewing. What possibly could have happened? Removal of the cracked crown hurt a lot, did that traumatize the tooth? Few weeks gone by and it still causes pain. ???
Charlene K
Reply –
We’re not going to have any specific answers for you but we do have several pages to refer you too. Possibly they can shed light on what you’ve experienced, either as an answer that you can figure out or in preparation of asking your dentist questions.
Only as a background reminder for other people reading, the outcome of performing dentistry can never be totally predictable. And for that reason any steps taken, like replacing large fillings with crowns, needs to have good justification. In Charlene’s case, it seems there was.
It’s disheartening to hear that your crown broke. Different types of crowns offer different success rates in regard to this point. Although, after an initial period, crown success can evidently become more predictable with all types.
There could be some simple explanations for the heat/cold sensitivity and chewing pain you notice.
1) A first check would need to be that the “bite” of the crown is precisely correct. (In theory, an error here might explain all of your symptoms.)
2) Thermal sensitivity with a crown might be explained by this phenomenon. (Use the link.)
Clearly your tooth needs to be evaluated by your dentist. No doubt they will first try any and all simple measures they can to resolve your issues, and then if they persist, continue on investigating from there.
In light of the fact that your tooth has an extensive history of potentially traumatizing events (large filling placement, cracks, repeated procedures), aspects of this page about the relationship between dental crowns and a need for root canal work might apply if the simple measures above don’t pan out.
Finally, what you report doesn’t jive precisely with what’s expected if the event that broke the crown further cracked the tooth. But no doubt your dentist will at least consider these issues too when evaluation your tooth.
Staff Dentist
Comment –
Replacing pfm crowns.
Recently my dentist placed 2 crowns in upper back teeth due to wear on my teeth. He wants to continue with his plan of treatment to replace previous crowns done in the past that are pfm because they are pfm and I was told that there’s no way to tell if they have decay under them and if they decay I’ll need an implant. Is it usual to replace for this reason? I’ve prob had them 10 years. I’ve not had a problem with them at all.
Rhonda
Reply –
In regard to tooth decay, there’s nothing usual or ordinary about a dentist replacing an existing PFM (or any type of crown) without cause or at least some level of suspicion.
—
New decay associated with a previously restored tooth is referred to as “recurrent” decay.
—
With an existing crown, recurrent decay could form on the tooth at the edge of the crown, and then continue on underneath it.
With this scenario, a dentist would typically identify the decay by feeling around the edges of the crown with a pointed dental instrument (an explorer).
If when pressed, if the explorer sticks into soft decayed tooth structure, or if the instrument detects a minute space (opening) between the crown and tooth (because of tooth structure loss due to the decay process) a diganosis of recurrent decay would be made. (By the way, since this type of cavity lies at the edge of the crown, signs of it quite possibly would show on an x-ray.
—
Or recurrent decay could form as a result of an “open margin.”
This is the situation where the fit of the crown on the tooth doesn’t create the seal that’s required. (A minute opening exists at the edge of the crown that extends on underneath between the restoration’s interior surface and the tooth nub it covers over.) (Why the open margin exists, or exists now, is too involved for this explanation.)
When an open margin is present, bacteria can seep into the creavas that exists and cause decay (up underneath the crown). This is a location where the decay that’s present probably wouldn’t be obvious on an x-ray.
—
So in your case, you would expect to hear your dentist say something like they found a “stick” (soft spot of decay) in association with your crown, or else mention that an “open margin” exists.
Short of that, a dentist might have strong suspicions about the presence of decay simply based on dark staining that now exists around the edges of the crown (tooth structure is white or yellow, darkened tooth structure can hint that adjacent (under the crown) tooth structure is decaying).
—
Ask your dentist to explain their reasoning more thoroughly. Maybe that will make the basis of their recommendation clearer to you, one way or the other.
Staff Dentist
Comment –
Front crown off.
Front upper crown has snapped off with remaining tooth. Can the crown be fixed back on
DH
Reply –
Look inside the crown. If it is 100% filled with tooth structure (or substantially close to it, or if the broken tooth structure comes to the edge of the crown in some location), possibly not.
The edges of a crown should overlap its tooth (Google “crown ferrule”). A ferrule design aids with crown retention. This area is also the aspect of a crown that creates its seal over the tooth (the seal being that which prevents oral fluids, microorganisms and such from seeping past/underneath the crown or into tooth spaces).
Even if a ferrule exists, the crown’s potential for long-term stability maybe compromised. (A crown’s stability in part depends on the shape and extent of the tooth structure that it fits over, much of which may now be missing.)
So bottom line, your dentist needs to examine your crown and the way it fits on your tooth to know if it can still be used.
If a very large percentage of the tooth inside the crown has broken off, the best, most-predictable solution may be (probably is) to remake the crown. If only a small amount of tooth structure has broken off, its loss may not be of any consequence. Sometimes the amount of tooth structure that has broken off lies in between, and while not entirely ideal, the adhesive nature of the cement that can be used aids with the the crown’s retention enough that from a practical standpoint makes a workable solution. Good luck.
Staff Dentist
