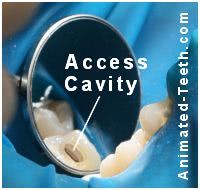
Creating the Access Cavity for a tooth’s root canal procedure.
What is a root canal “access cavity”?
As a starting point for performing your tooth’s endodontic therapy, your dentist must gain entry to the nerve space inside your tooth. The process of using a dental drill and making this opening is termed creating an “access cavity.”
The space inside your tooth that the opening gives access to is its pulp chamber and root canals. And this is the area inside your tooth that will be treated during its endodontic procedure.
An access cavity must meet two important goals.
While making the opening in your tooth, your dentist will focus on two main goals.
The access cavity must provide adequate access to all portions of the tooth’s interior …
(Both from the standpoint of being able to see inside the tooth and providing adequate physical access for the instruments and materials that the dentist will use during your root canal procedure.)
… but not result in the removal of any more sound tooth structure than is absolutely necessary.
(Removing excess tooth structure will tend to weaken the tooth or unduly complicate rebuilding it after its procedure has been completed.)
So, as you can see, creating this opening properly plays an important role in helping to ensure the success of your tooth’s procedure, both on a short and long-term basis.
▲ Section references – Tronstad
The steps of creating an endodontic access cavity.
Note: This step marks the formal beginning of your tooth’s root canal procedure The steps.. As such, it’s only begun after your tooth has been properly numbed up What to expect. and then isolated by way of placing a rubber dam. Why this is important.
Note: A rubber dam has been placed.
Step #1: Choosing the opening’s location.
A primary characteristic of an access cavity is it must provide straight-line access to the tooth’s individual root canals.
Why straight-line?
a) So the dentist’s instruments can be inserted.
Root canal files Details. | Pictures. are long, straight, pin-like objects and it takes a relatively straight path to be able to insert them into a tooth and its root canals.

Straight-line access is needed to insert a file into a tooth’s root canal.
b) So the dentist’s instruments can be used properly.
As a file is worked up and down inside a canal, any portion of the tooth that deflects its motion will affect the way it cuts and contours the walls of the tooth’s root canals. Unencumbered straight-line access helps the dentist avoid the complications that this hindrance can create.
So, where on a tooth is the access cavity made?
Due to the above requirements, and based on the anatomy of the root canal systems of teeth:
- With back teeth (molars and premolars) – The access cavity is created on the occlusal (chewing) surface of the tooth.
- With front teeth (incisors and canines)- The opening is made on the lingual (backside) surface of the tooth.
And while there can be exceptions to these general rules, for the vast majority of cases this is where the opening is made.
Step #2: Making the access cavity.
It’s a simple matter for your dentist to create a hole in your tooth. They’ll simply use their dental drill, not unlike when they prepare a tooth for a filling.
What will they find inside your tooth?
The area your dentist is trying to reach is your tooth’s pulp chamber. With normal healthy teeth, this area is filled with live pulp tissue (tooth nerve tissue).
What remains of the pulp when a root canal procedure is needed and performed will vary. It might still be “vital” (live nerve tissue is present), be “necrotic” (the nerve has died), or have some status in between.
A tooth’s pulp chamber is a hollow space. The dentist may or may not find it filled with nerve tissue.
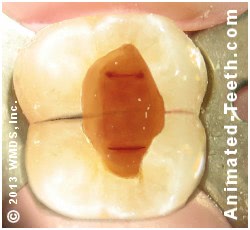
The openings into the tooth’s root canals can be seen on its floor.
Your dentist’s goals as they craft the access opening.
As they develop the access cavity’s shape and contours, your dentist will keep several issues in their mind.
- Does it reveal the locations where the tooth’s root canals can be expected to be found?
- Does it provide the needed straight-line, unencumbered access to them?
- Does it remove aspects of the tooth’s pulp chamber that might serve as a harbor for debris and contaminants?
Additional issues and requirements.
All tooth decay must be removed from the tooth.
Tooth decay harbors bacteria and assorted debris and these contaminants must be removed from the tooth.
Notice how one side of this tooth is missing.

The tooth’s filling and the cavity that undermined it were removed when its access cavity was made.
All fragile and/or loose portions of the tooth must be removed.
This includes both portions of the tooth and its dental restoration if there is one. Leaving structurally sound portions of a tooth’s existing dental restoration is common.
The main goal here is simply one of predictability. The dentist needs to know that what exists will remain intact (won’t fracture or break off) during the tooth’s root canal procedure or between appointments.
What about making the access cavity directly through a tooth’s existing dental crown?
Doing so is common. However, there are several important issues and considerations associated with making this choice.
For more details, visit our page: Performing root canal treatment on teeth that already have a crown. Can the crown be reused?
What is making the access preparation like for you (the dental patient)?
As mentioned above, a dentist doesn’t start the process of creating the tooth’s access cavity until after it has already been numbed up. So you shouldn’t feel anything, at least of any significance.
What will you feel?
The local anesthetics (“shots”) used in dentistry are characteristically only effective in preventing the sensation of pain, not pressure. So you can expect to feel the vibrations that your dentist’s instruments create as they are used.
- You’ll notice the light vibrations of their “high speed” drill as it’s used to initially penetrate through your tooth’s hard enamel layer. (Exactly like you would feel when having a filling placed.)
- Once the general size and shape of the access cavity have been developed, your dentist will likely switch out the type of handpiece (drill) they use to a “slow speed” one (like when they widen and flare the individual openings of each root canal). These drills tend to create a slower, sometimes heavier, level of vibration.
For most people, that’s about all that will be noticed.
What might you feel?
While this isn’t the usual course of events, we think it’s important to mention that with some types of cases, and some scenarios, the potential for the patient to feel pain does exist. We discuss this issue on this page: Does having root canal treatment hurt? Polling from studies.
Because of this potential, it only makes sense that at the onset of a patient’s appointment, they establish with their dentist some type of sign that indicates that a problem has been noticed. That way the dentist will know to stop immediately and tend to it. The use of a predetermined hand signal is common. A smart move.
Step #3: Refining the access cavity’s shape.
When the process of creating a tooth’s access cavity has been completed and when its next stage of treatment has been begun (cleaning and shaping its canals The steps.) isn’t clear cut.
That’s because the opening’s shape will be continually refined as each new need is identified during its procedure.
- If during the tooth’s treatment the potential for additional canals is suspected, the access cavity may have to be enlarged when searching for them.
- While instrumenting a canal, if the dentist finds that the confines of the opening restrict the file’s freedom (as discussed above), they’ll simply trim that portion of the tooth back.
Adjustments like these should take just a few moments to accomplish and be a non-event for the patient.
Complications associated with access cavities.
Root perforations.
Making an initial opening in a tooth and then expanding it so it reveals the opening of each of the tooth’s root canals isn’t always an easy, straightforward task.
As examples, sometimes instead of being hollow, the tooth’s pulp chamber is substantially calcified. Or some of the tooth’s root canals may not join with the chamber in the expected locations.
Difficulties for the dentist.
When an atypical situation exists, the dentist will need to use their drill inside the tooth more extensively. And as they continue to trim away more and more of the internal aspect of the tooth, knowing how close they are getting to the root’s outer surface is impossible to know precisely.
(With challenging cases, the landmarks inside a tooth that are routinely relied upon as reference points may not, or may no longer, exist. Also, with a rubber dam in place, understanding the orientation of a severely broken-down tooth can be quite difficult to interpret. With each of these scenarios, the dentist’s drill may not be trimming precisely where they expect.)
Perforations.
When dealing with these types of difficult cases, the dentist’s drilling as they create the access cavity may result in the creation of a perforation (a hole that extends out the side of the tooth’s root).
Treatment.
The extent to which this is a problem will have to be evaluated by your dentist. In some cases a successful repair is possible.
A case’s prognosis will typically depend on the size and location of the opening, when it was diagnosed and treated, and the materials used to make the repair. MTA (mineral trioxide aggregate), a biocompatible compound high in calcium and phosphorus, is currently considered the material of choice.
Smaller perforations, located further down on the tooth’s root, tend to offer a more favorable treatment prognosis. Also, perforations that are identified and treated promptly (a strategy that helps to prevent secondary inflammation and eventual infection of the tissues surrounding the site) tend to have a more favorable outcome.
▲ Section references – Ingle
Excessive tooth structure removal.
With every case, the dentist’s goal will be one of keeping the overall size of a tooth’s access cavity as conservative as possible.
The challenge.
Once a tooth’s endodontic work has been completed, it will need to be restored. And making an access opening that’s oversized might make doing so more difficult. Also, removing an excessive amount of tooth structure could conceivably weaken the tooth. How crowns strengthen teeth.
That’s not to say that all access cavities should be “small.” Instead, and simply, no preparation should be larger than the dentist determines is necessary to perform the tooth’s work successfully.
Not all access preparations can be kept conservative.
Few teeth that end up requiring root canal treatment are pristine. Most have been affected by some type of trauma (e.g. extensive tooth decay, fracture).
Since the creation of an access cavity always includes removing all tooth decay and may include removing the tooth’s current restoration too, some access openings will necessarily wind up encompassing a large portion of the tooth.

This access cavity is very large because tooth decay and the tooth’s filling needed to be removed.
Rebuilding the tooth.
What remains of the tooth will dictate what type of final restoration should be placed, such as a dental crown vs. a filling.
It’s important to note that the choice that’s made can have a substantial impact on the long-term success of the tooth’s procedure. We discuss this issue in detail on our page: Rebuilding your tooth after its root canal treatment. Options.
What’s next?
We have more to share about having root canal therapy.
Page references sources:
Ingle JI, et al. Ingle’s Endodontics. Chapter: Preparation of Coronal and Radicular Spaces
Tronstad L. Clinical Endodontics. Chapter: Preparation for treatment.
All reference sources for topic Root Canals.
