Root canal treatment aftercare and recovery.
Following your root canal treatment …
Once your dentist has finished your tooth’s endodontic therapy (or even if you’re just between root canal appointments) you’ll no doubt want to know what to expect during the recovery process that follows. That includes both immediately (the day of your procedure) and also over the next several days.
Additionally, you’ll need aftercare instructions covering what you can do, should do, and should not do during your recuperation. Adhering to these directions is important because they will help your tooth’s healing process progress as quickly as possible and help you avoid complications.
On this page, you’ll first find a brief outline of the dos and dont’s you should follow during these time periods:
- Immediately following your tooth’s root canal procedure (same day).
- Over the next several days.
- Long-term aftercare.
Following those instructions, we provide more detailed information about the following subjects:
- Precautions to take with your just worked-on tooth. – Things to watch out for and why.
- Rules about eating – What kinds of foods and beverages? How soon?
- Maintaining proper oral hygiene – Brushing, flossing, rinsing.
- Post-operative pain – What to expect. / Causes. / Pain management. / Prevention.
Some background about root canal therapy. –
In case you don’t know …
What your tooth has been through may affect certain aspects of its aftercare and recovery. So, briefly, here’s some background information about endodontic therapy, like why it’s needed and what takes place when it’s performed.
a) What is a Root Canal?
Root canal therapy is a procedure dentists perform to save teeth that have advanced nerve-space complications from requiring tooth extraction.
Performing it provides a way of preserving your natural teeth (like for proper chewing function and aesthetics). Alleviating pain and/or remedying swelling the tooth’s condition may have caused. And it prevents the tooth from creating future complications, like abscesses or bone tissue damage.
b) Why is a root canal necessary?
Certain types of events can compromise the health status of a tooth’s pulp (nerve tissue). As examples, advanced tooth decay, cracks, or trauma can lead to pulp tissue inflammation, infection, or even death. And these kinds of nerve tissue changes can lead to pain, tooth infection, and swelling.
During root canal therapy, the diseased pulp tissue (and any associated bacteria and contaminates) are removed from within the tooth’s nerve space. This area is then disinfected and filled in (sealed). Doing so both alleviates the tooth’s current problems (infection, pain, swelling) and prevents future infection of this space.
c) How is the root canal procedure performed?
Using a series of specialized instruments, your dentist will first remove all remnants of your tooth’s pulp tissue (along with accumulated bacteria and associated debris) from within your tooth (its pulp chamber and root canals).
This work, in conjunction with periodically flushing your tooth with an appropriate solution, will disinfect its nerve space.
The cleansed space is then filled in using a biocompatible material termed gutta-percha. The seal it creates prevents future reinfection of your tooth’s interior.
Aftercare Instructions:
Dos and don’ts for specific time frames following your procedure.
1) Root canal aftercare immediately following your tooth’s procedure.
The anesthetic (local anesthetic, dental shot) you’ve been given for your treatment will stay effective for some hours following your appointment. And this continued numbness will need to influence many aspects of what you should and should not do during this aftercare period.
a) Eating.
Immediately following your procedure, you should limit your eating activities until that point when your numbness has finally worn off and your ability to feel sensations fully has returned.
- Failing to do so could result in damage to your tooth, like the case where you might chew or bite down on it heavily by mistake. (Root-canalled teeth are typically fragile and prone to breakage until their final/permanent restoration has been placed.)
- Trying to eat while numb may result in your accidentally biting your tongue or cheek.
- If you can’t wait, any foods that you do eat should be soft and preferably ones that don’t require much chewing. (Smoothies, yogurt, or mashed potatoes all make good choices.)
- The temperature of all foods and beverages should be monitored so you don’t burn yourself while numb.
Later on.
Once your numbness has finally worn off, eating is OK. But softer foods still make the best choice and keep food, and especially any that requires chewing, on the side opposite your root canalled tooth.
FYI: More dos and don’ts about eating after your root canal procedure Go
b) Pain.
If at the completion of your appointment your dentist has made a recommendation about taking pain relievers (prescription or over-the-counter), starting them while you’re still numb may make a good plan. That way the medication can start to produce its effect as your anesthetic (numbness) gradually wears off.
This plan is especially favorable for anti-inflammatory analgesics (like ibuprofen/Motrin/Advil, NSAIDs). Starting this kind of medicine immediately (as directed) can help to limit the inflammation reaction triggered by your procedure and therefore the level of pain you ultimately experience.
FYI: More details about post-procedure pain and managing it Go
c) Antibiotics.
If your dentist placed you on antibiotics before your procedure, even now with your appointment completed, you should continue to take this medication as originally directed.
2) Root canal aftercare during the next few days.
a) Pain management.
It’s normal and expected that a patient may experience some discomfort with their tooth following its root canal procedure. In most cases, the pain that’s felt is a result of an inflammation reaction triggered by their tooth’s work.
Pain remedies.
When appropriate for a patient’s use, taking an over-the-counter (OTC) anti-inflammatory analgesic (an NSAID, like ibuprofen/Motrin/Advil) makes a good choice for controlling this kind of discomfort. NSAID compounds are not only good pain relievers but are also effective in limiting inflammation (the process that’s triggered the pain that’s felt).
FYI: More details about post-procedure pain and managing it Go
b) Eating.
During the several days following your root canal treatment, you should take it easy with what you eat so you don’t irritate or possibly even damage your healing tooth.
- Choosing soft foods makes the best plan. Scrambled eggs or oatmeal for breakfast and things like meatloaf with mashed potatoes or else a pasta dish for lunch or dinner all make good choices.
- Do your biting and chewing on the opposite side from where your work was done. Excessive forces, like those created when eating hard or crunchy foods, can traumatize a healing tooth.
Additionally, root-canalled teeth are often fragile and prone to breakage until their final/permanent restoration has been placed. Keeping your eating activities away from your tooth can help to avoid this complication.
- Besides just hard foods, avoid sticky ones too. They may pull out your tooth’s temporary filling or crown. Avoid chewing gum too.
FYI: More dos and don’ts about eating after your root canal procedure Go
c) Oral home care.
Maintaining good oral hygiene will help your tooth and its surrounding tissues recover as quickly as possible from its root canal procedure.
- Expect that the gums around your tooth may be tender and sensitive (they’re often traumatized by the rubber dam clamp that was placed). Make sure to use a soft-bristled toothbrush so you don’t irritate these healing tissues. Rinsing with warm salt water a few times a day will help them heal faster.
- Ease back into your flossing routine but make sure to be gentle. Also, your tooth’s temporary filling or crown may not meet the same high standards that permanent ones do. As you floss, if your floss seems to want to get stuck, let go of one end and then just pull it out to the side.
FYI: More dos and don’ts about brushing and flossing after a root canal Go
d) Antibiotics.
Even though your tooth’s endodontic therapy has been completed, any antibiotics prescribed by your dentist should continue to be taken as directed.
3) Long-term aftercare following a root canal.
The most important thing to understand about long-term aftercare is that even though your tooth’s root canal therapy has been completed it still requires additional dental work and monitoring.
a) Placing your root canalled tooth’s permanent restoration.
All teeth that have had root canal therapy will need some type of final (“permanent”) restoration placed. And until it has, the tooth should be considered fragile and prone to breakage. Any damage that does occur may lead to root canal treatment failure or worse, the tooth may require extraction.
The kind of permanent restoration that’s chosen (filling, crown), as well as the time frame in which it’s placed, can greatly influence the long-term success of a tooth’s completed endodontic work. Use this link for a discussion about the different kinds of final restorations that might be chosen. Which is best?
b) Follow-up appointments.
It’s important to keep any follow-up appointments your dentist feels are necessary to schedule. During these checkups, your dentist will examine your tooth and evaluate its healing progress (taking X-rays will probably be required). They will also evaluate your surrounding gum tissue for any signs of persistent infection or inflammation.
Further details about root canal aftercare.
Besides just instructions about what you should or shouldn’t do, if you’re curious about the reasons that lie behind endodontic recovery dos and don’ts (like why the potential complication exists or why its remedy works), read on.
- Taking precautions with your just-treated tooth.
- Needed rules about eating.
- Maintaining proper oral hygiene.
- Post-procedure pain – What to expect. / Causes. / Pain management. / Prevention.
1) Following your treatment, be careful with your tooth.
Don’t look for trouble. It’s best to exercise caution with any tooth that’s either in the process of having endodontic therapy (like with multiple-vist cases) or has just had it completed.
Favor your tooth.
Until its permanent restoration has been placed, you should avoid using your root canalled tooth very extensively. You don’t want to take any chances because …
a) Its temporary filling may break.
For completed root canal therapy …
As a final step of your tooth’s procedure, your dentist will place a temporary dental filling to protect their completed work until that point in time when a final/permanent restoration can be placed. (Possibly a filling. Some teeth require dental crowns.)
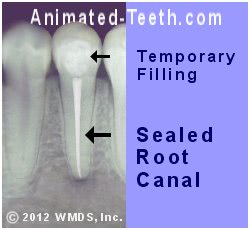
Temporary filling placed at the completion of root canal treatment.
If you subject your temporary filling to heavy use or excessive force, it may break. If so, the protective seal it creates will likely be lost and saliva and debris (and all of the bacteria and contaminates they contain) will be able to reenter your tooth.
As a worst-case scenario, this seepage may reinfect your tooth’s just-treated root canal space and therefore its endodontic work will need to be repeated.
Dentists refer to this complication as coronal leakage Explained. and this issue is a primary reason why upon the completion of your tooth’s endodontic work its permanent (final) restoration should be placed as soon as can reasonably be arranged.
For two-visit root canal cases …
In cases where your tooth’s treatment requires more than one appointment to complete What decides?, if you overuse the temporary filling that’s been placed to protect your root canal work between visits, it might break or come out completely.

Temporary filling placed between root canal appointments.
If the filling breaks, saliva, and debris (and the bacteria and debris they contain) will recontaminate the interior of your tooth. If so, your dentist will have to spend your next appointment cleaning out your tooth a second time (a repeat of your first visit). Your treatment will probably end up taking more visits than originally planned.
b) Your tooth may break.
The temporary filling that’s been placed at the completion of your root canal treatment provides very little if any structural reinforcement for your tooth (that’s one purpose of placing a “final” restoration). While in this fragile state, extensive use of your just-treated, temporized tooth may lead to breaking or cracking.
Two major issues of concern are:
- Tooth breakage may compromise the seal of the temporary filling that’s been placed and therefore allow oral contaminates and bacteria to reinfect the treated nerve space inside your tooth. If so, its root canal therapy will need to be performed again.
- Extensive tooth fracture, and especially the formation of root cracks, may render the tooth irreparably damaged. If so, it will need to be extracted.
After root canal treatment, since their tooth feels back to normal, a person is often eager to start using it again. But until your dentist has had a chance to place its final/permanent restoration What will be needed?, it should be considered fragile.
2) Precautions with eating after root canal treatment.
a) Hard foods may cause breakage.
In light of the information we’ve just explained about the potential for tooth or temporary restoration damage/breakage and the complications that result, it should be obvious why during your tooth’s recovery (and all of the way up until its final/permanent restoration has been placed) you should avoid biting into or chewing on hard or crunchy foods. This includes things like raw carrots or celery, hard candies, and nuts.
Additionally, sticky foods (like taffy or caramels) and chewing gum should be avoided for fear of pulling loose your tooth’s temporary filling or crown.
As a general rule, until its permanent restoration has finally been place, always shift your food and do your chewing on the opposite side from your root-canalled tooth.
b) Opt for soft foods.
Choosing softer foods during root canal recovery always makes the better choice. Pick foods that are easy to chew and won’t place excessive pressure on your tooth.
Things like soup, pasta, meatloaf, fish, mashed potatoes or other vegetables, yogurt, cottage cheese, and fruit smoothies all make good choices.
c) Avoid eating while numb.
Immediately following your root canal procedure, you’ll still be numb for several hours. And trying to eat during this period of lost sensation can lead to complications.
- While numb, you may inadvertently chew on or bite heavily on your treated tooth thus damaging it or its temporary restoration.
- Your numbness may lead to accidentally biting your tongue or cheek while chewing.
- Consuming extremely hot foods or beverages when numb places you at risk of inadvertently burning your mouth.
3) Maintaining proper oral home care.
Maintaining proper oral home care is important for any tooth, including one that’s had root canal treatment.
- Immediately after your treatment, go ahead and settle back into your normal brushing routine. But as you brush make sure to be gentle because the gum tissue around your tooth may be irritated from the rubber dam clamp that was used during your procedure. Using a soft-bristled toothbrush can help.
- Gargling with salt and water three times a day can help promote the healing of traumatized soft tissues. Mix 1/2 teaspoon of salt into warm water. Swish it in your mouth for about a minute and then spit it out.
- There are some special concerns about flossing. We discuss them next.
Tips on flossing a root canalled tooth that still has a temporary filling or crown.
The temporary filling or crown that’s placed at the completion of your tooth’s root canal procedure may not be as finely crafted as the permanent one that will be placed later. For example, take a look at the two restorations shown in our graphic below.
- Restoration “B” represents a “permanent” filling that’s been placed in a tooth following its root canal treatment. Notice how its contours align smoothly with the sides of the tooth.
- Restoration “A” represents a temporary restoration, and notice how its contours extend past the side of its tooth. These ledges are referred to as “overhangs.”
What to watch out for when you’re flossing.
In the case where a temporary restoration has an overhang, when you floss it may snag this ledge and end up pulling your restoration out. So, as you floss …
- If your floss feels like it’s starting to get caught, back off. Forcing your way may end up with getting your floss stuck or breaking your filling.
- If you get into trouble or are close to it, let go of one end of your floss and then pull it out to the side.
- Despite the temporary nature of this restoration, report the difficulties you’ve noticed to your dentist so they can trim off the overhang.
(If you can’t clean your gums around your tooth properly they will become tender and sore. Poor gum health will also make the process of creating the final restoration for your root-canalled tooth more difficult.)
4) Discomfort following a root canal – What to expect.
a) Will you have any pain after your root canal appointment?
It’s a disappointing fact but some percentage of people will experience some level of discomfort after their root canal work, to the point of it being a normal and anticipated postoperative complication.
b) Does having post-op pain indicate that your root canal treatment has failed?
Feeling discomfort immediately following your endodontic therapy and even for some days beyond is not a negative indicator of the outlook for your treatment’s long-term success.
c) What are the chances that you’ll experience pain?
It’s generally reported in dental literature that somewhere between 40% to almost 60% of patients will experience some level of discomfort after having had endodontic treatment. It’s important to keep in mind however that these numbers include all cases lumped together, ranging from very slight to the most severe.
d) How much pain can you expect?
A number of studies have evaluated this subject. As examples:
Study #1 – Sadaf (2014)
This study gives some overall insight into what can be expected.
- This study monitored 140 patients during the day (24 hours post-op) following the completion of their (two-visit) root canal therapy.
- 57% reported no discomfort after their work. For those who did, 22% reported mild, 19% moderate, 1% intense, and 1.4% unbearable pain.
Comment – These findings parallel the 40% post-op pain number cited above (43% did experience discomfort). But they also reveal that roughly 80% of patients either experience just minimal or no pain.
Study #2 – ElMubarak (2009)
A second study we’ll mention was performed by ElMubarak. It monitored patients completing their endodontic treatment (requiring either 1 or 2 visits) at points 12 and 24 hours post-op.
The findings were somewhat different than those reported by Sadaf. With this study, both time intervals shared similar numbers:
- At 24 hours – 89% developed no discomfort. 2% experienced mild, 1% moderate, and 9% severe postoperative pain.
Comment – In a positive light, over 90% of patients had just minimal or no pain. Although admittedly, almost 1 in 10 experienced significant discomfort.
▲ Section references – ElMubarak
Study #3 – Ali (2016)
A study by Ali followed 270 patients who underwent one-appointment endodontic therapy for up to 72 hours following their treatment. Of these patients:
- 55% experienced some level of postoperative pain.
- Broken down into groups: 26% of patients experienced slight pain (no analgesic needed), 21% moderate (pain relievers were required), and 7% severe discomfort.
Comment – This paper was clear to point out that the occurrence of postoperative pain of low to mild intensity is common, even in cases where the patient has experienced no prior pain with their tooth and/or despite the dentist following acceptable standards of treatment.
e) What to expect over longer time frames.
As a further example of what you might expect postoperatively, a study by Al-Negrish followed a group of 112 patients for a period of one week after the completion of their root canal therapy. If determined:
- At two days post-op: 80% of patients had no pain, 8% had slight pain, and 12% had moderate to severe pain.
- By day 7: 93% of patients had no pain, 4% had slight pain, 3% had moderate pain and one was experiencing severe pain.
Comment – It would be our interpretation that collectively, all of the studies cited above on this page suggest that while problems can occur, for the vast majority of people their endodontic work is completed with just mild or no postoperative symptoms (over both the short and long-term).
▲ Section references – Al-Negrish
f) What type of pain can you expect following root canal work?
What’s common –
- The discomfort typically starts within a few hours after your root canal appointment.
(Premedicating with an OTC pain reliever may help to minimize the level of pain you experience. Discussed here.)
- The pain may persist for several hours up to several days.
- The severity of the discomfort gradually decreases over time.
▲ Section references – Makhtari, Sadaf
While you should always feel free to contact your dentist whenever you have concerns, experiencing any of the following issues should definitely prompt you to do so.
Reasons to contact your dentist –
- Severe pain or a sense of pressure that lasts for more than a few days.
- The development of swelling inside or outside your mouth.
- Symptoms return that are similar to what you experienced prior to your treatment.
Additional reasons to contact your dentist –
- Your bite on the treated tooth feels uneven (see below).
- The temporary crown or filling that’s been placed on your tooth has dislodged.
- Experiencing an allergic reaction to medications you’ve been given or have taken is possible. Watch for signs such as itching or the formation of a rash or hives.
5) What causes after-root canal treatment pain?
a) The discomfort you notice is probably due to inflammation.
The most common source of pain after root canal treatment is inflammation of the tissues that surround the tooth’s root (termed “periradicular inflammation”). They may be irritated by any and all of the following types of events.
Overinstrumentation is a common cause of post-treatment pain.
- Root canal files that have poked beyond the end of the root. This is referred to as “overinstrumentation” (see animation).
(This is why one of the first steps of root canal treatment involves measuring each canal’s length. How that’s done. The dentist’s goal will then be to stay within the confines of these measurements Using markings found on each file. as they perform the tooth’s work.)
- The escape (extrusion) of bacteria and debris from the root’s tip.
- Leakage of solutions and medicaments used during the root canal process from the tooth into the tissues surrounding its root.
These events aren’t necessarily preventable.
It’s important to point out that despite a dentist’s best efforts to minimize the chances of each of the above from occurring, being able to absolutely prevent them is something that lies far beyond their control.
b) Infection may play a role.
It’s possible that the process of performing a tooth’s root canal therapy has triggered the activation of bacteria living in association with it. If so, an acute infection may develop.
But in the majority of cases, the discomfort a person notices after their appointment is primarily due to tissue inflammation without the complication of active infection.
What might trigger post-op infection?
The general scenario involved is one where during the cleaning and shaping process How this is done. the action of the dentist’s files within the tooth’s root canal(s) results in the escape of bacteria into the tissues that surround its root(s).
Studies have shown that despite their best efforts, the extrusion of debris from a tooth during cleaning and shaping tends to occur regardless of the technique the dentist uses (Sipaviciute). We’ll also mention that it would be impossible for the dentist to know if, or to what extent, this event had taken place.
Whether or not what has occurred will trigger a significant event is quite variable. Factors such as the virulence of the microorganisms involved, their numbers deposited in the root’s surrounding tissues and the effectiveness of the person’s immune system in response to them will all play a role.
c) Other possible causes of pain after a root canal.
a) Gum tissue trauma.
During each root canal visit, your dentist will isolate your tooth by placing a rubber dam (a thin sheet of latex) around it. The prongs of the metal clamp used to hold it in place may cause minor gum tissue irritation. Remedy
b) A high temporary filling.
If the “bite” of the filling that your dentist placed at the completion of your dental visit is too “high” (too tall, in the sense that when you close down you strike the filling first), your tooth may become traumatized and begin to hurt.
- The needed solution is that you return to your dentist’s office so they can buff the filling down until its bite is correct.
- Since this trauma causes inflammation of the tissues that surround the tooth, even after the filling has been trimmed the pain may continue for some time.
The inflammation management techniques discussed above would be appropriate for this problem too.
▲ Section references – Ingle, Sipaviciute
Predictors of experiencing pain after root canal work.
There are some risk factors that tend to correlate with which patients will or won’t experience discomfort after their root canal appointment.
Preoperative pain = Postoperative pain.
A study by Sadaf (linked above) determined that the biggest risk factor for postoperative discomfort is having preoperative pain. 83% of patients whose tooth hurt prior to their root canal appointment experienced pain afterward. In comparison, only 17% of those without symptoms did.
As lesser factors, this study also determined that:
- Females are more likely to experience discomfort (65% vs. 35% for males). (Other studies have reported similar findings.)
- Possibly the type of tooth receiving treatment is a factor. In this study, 50% of patients experienced moderate pain when a lower molar was treated vs. 35% for upper ones. Lower numbers were associated with other types of teeth. (Not all studies have found tooth type to be a relevant factor.)
Other studies have reported similar findings.
Ali (linked above) evaluated the postoperative pain experienced by 270 patients following single-visit endodontic therapy.
- 69% of patients who had no preoperative pain remained pain-free following their tooth’s procedure.
Of the group that did have preoperative pain, 100% also experienced postoperative discomfort.
- Only 4% of the no pre-op pain group experienced severe post-op pain.
73% of the group that had pre-op pain had severe post-op pain.
- This study also determined that the treatment of premolar and molar teeth was more likely to be associated with postoperative pain than front ones. And that treating lower teeth resulted in post-op pain more so than uppers.
6) Managing post-root canal pain.
Since the most likely cause of discomfort after a root canal appointment is periradicular (around the root) tissue inflammation (see above), a dentist’s initial treatment is typically focused toward managing it. A paper by Jayakodi discusses the following treatment approaches.
Note.
Whenever a medication is selected for use, the patient must evaluate the product’s labeling to make sure its use is appropriate for them. The product’s dosing recommendations should not be exceeded.
NSAID analgesics.
Dentists frequently use over-the-counter (OTC) “nonsteroidal anti-inflammatory drugs” (NSAIDs) as their first choice in treating tissue inflammation triggered by root canal work.
Ibuprofen (Motrin, Advil) is typically the drug selected. The use of an NSAID alone is usually sufficient for what most patients experience.
Dosing.
For healthy full-sized adults (with no complicating factors and under the guidance of their dentist), a common regimen is: 200 to 400 mg orally every 4 to 6 hours as needed for pain relief.
Acetaminophen.
In cases where the use of an NSAID cannot be tolerated by the patient (known sensitivity to NSAIDs or aspirin, gastrointestinal ulcerations, NSAID complicated hypertension), a dentist will typically turn to the use of acetaminophen (Tylenol).
Dosing.
For healthy full-sized adults (with no complicating factors and under the guidance of their dentist), a common regimen is: 325 to 650 mg every 4 to 6 hours as needed for pain relief.
Prescription medications.
If the patient’s pain can’t be controlled by one of the above drugs, a narcotic analgesic (prescription pain reliever) may be required. It’s sometimes given in combination with an NSAID.
Antibiotics.
As stated above, tissue irritation as opposed to active bacterial infection is the most common cause of a patient’s pain after root canal therapy. And for that reason, the initial treatment of what a dentist interprets as a routine case typically won’t include the use of an antibiotic.
If at any time they have reason to suspect that infection does play a role, an antibiotic will be prescribed.
Keep in touch with your dentist.
It should go without saying that in all cases where you are experiencing any type of problem, you should always feel free to contact your dentist. They are familiar with the statistics above and fully expect that some percentage of their patients will require their assistance.
▲ Section references – Jayakodi
7) Preventing anticipated post-root canal treatment pain.
Before your appointment.
“Premedicating” with an NSAID before root canal work may help to limit or prevent the amount of postoperative discomfort a patient experiences. Ibuprofen (Motrin, Advil) is frequently used. Ask your dentist what makes an appropriate choice and plan for your case.
A study by Mokhtari determined that a single 400mg dose of ibuprofen one hour prior to the patient’s appointment was effective in reducing pain over the first 8 postoperative hours.
▲ Section references – Mokhtari
Following your appointment.
In cases where premedication with an NSAID before your appointment was not considered, per your dentist’s recommendation taking a dose before the local anesthetic used for your procedure has worn off can be effective in helping to prevent or limit post-endodontic treatment pain.
While the time frame involved is shorter than with premedication and therefore likely to provide a less pronounced benefit, the idea is that the NSAID can start to have an effect prior to that point when any pain can be felt.
What’s next?
If your tooth’s root canal treatment has been completed, the next step is rebuilding your tooth. Towards that goal, these pages should be of special interest.
- What kind of final restoration should be placed?
- Can an existing crown be used after a root canal?
- Dental post and cores? When is one needed?
Page references sources:
Al-Negrish, A. et al. Flare up rate related to root canal treatment of asymptomatic pulpally necrotic central incisor teeth in patients attending a military hospital.
Ali A, et al. Influence of preoperative pain intensity on postoperative pain after root canal treatment: A prospective clinical study.
ElMubarak AHH, et al. Postoperative Pain in Multiple-visit and Single-visit Root Canal Treatment.
Ingle JI, et al. Ingle’s Endodontics. Chapter: Treatment of Endodontic Infections, Cysts, and Flare-ups.
Jayakodi H, et al. Clinical and pharmacological management of endodontic flare-up.
Mokhtari F, et al. Effect of Premedication with Indomethacin and Ibuprofen on Postoperative Endodontic Pain: A Clinical Trial.
Sadaf D, et al. Factors Associated with Postoperative Pain in Endodontic Therapy.
Sipaviciute E, et al. Pain and flare-up after endodontic treatment procedures.
Tsesis I, et al. Flare-ups after endodontic treatment: a meta-analysis of literature.
All reference sources for topic Root Canals.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Pain after root canal.
I had a root canal yesterday morning and after the numbness wore off I realized that it still hurts just as bad or more than it did before. I talked to the dentist this morning and he said he felt the procedure went well so he’s not sure what could be causing the pain. He thinks maybe the infection still is bothering me so he prescribed another antibiotic to go along with the one I am already on. Any thoughts on why this tooth would still be hurting if the dentist is sure the procedure was successful?
DR
Reply –
As discussed above, a common cause of post-root canal pain is inflammation. The inflammation is your body’s response to irritation triggered by activities that occurred during the procedure, many of which are simply not preventable or are caused unknowingly by the dentist.
Also as discussed above, when appropriate for the patient, a dentist frequently has them take an NSAID medication for pain relief, frequently one that is available on an over-the-counter (OTC, non-prescription) basis.
Whatever is decided as the cause or the plan for relief, a dentist will usually feel (so check with them) that it’s important for a patient to continue to take their antibiotics as prescribed, to completion (meaning all of the pills/capsules originally dispensed are ultimately taken).
Staff Dentist
Comment –
Pain after initial filling of root canal
I experience a worse pain after initial appointment after temporary filling ….using medicines but after 3-4hours pain is recurring. ..no swelling noted….now its 2days already but still pain persists. ..i just started antibiotic. ..next appointment after 5days….what to do else???please reply
Sbinu
Reply –
Here’s some general information. We’re assuming of course that you have already been in contact with your dentist and sought their attention.
In general terms, the most common cause of post-root canal treatment pain is inflammation. In managing that, a dentist will usually rely on the use of NSAID medications.
If the chosen NSAID alone does not adequately control the patient’s pain as it’s helping to decrease and control the inflammation that exists, the dentist might consider the use of a prescription narcotic pain reliever. (Generally narcotics can be expected to provide a higher level of pain relief.)
The use of the narcotic might replace the NSAID, or else some type of combination therapy or combination product might be used where receiving the benefits of both types of medications are possible.
Less common is the situation where post-root canal pain is caused by active infection associated with the tooth. For the most part, the obvious signs associated with infections (swelling, indications on x-rays, pus venting) take time to develop, so making a diagnosis of this type of scenario can be difficult initially.
Unlike a pain reliever, when oral antibiotics are taken it generally takes a day or so for them to start to have much of an effect. (That’s why some antibiotic regimens start with a loading dose, and then a lower one for the remainder of the dosings.) While the antibiotic is creating its effect, the patient is kept comfortable via the use of pain relievers.
While not especially commonplace, shorter durations of relief might be provided by the dentist numbing up the patient’s tooth again (use of a local anesthetic, giving a dental shot). Long-lasting anesthetics (bupivacaine) can take several hours to wear off (6 or so).
There can be other possible solutions, needed treatments or management methods. But what the dentist needs the most is a diagnosis of what is the primary underlying cause of the pain so they can target their treatment directly toward that.
They can only make that determination via understanding your symptoms, examining/evaluating you and, unfortunately, seeing how your symptoms develop over time.
You state “… next appointment after 5days ….what to do else???”. We find it hard to believe that your dentist expects you to go 5 days unattended while having difficulties.
As the provider of your endodontic treatment, it’s your dentist’s obligation to help you through whatever treatment complications crop up. So be in touch with them. It’s the squeaky wheel that gets oiled. If they don’t continue to hear from you they will likely assume your symptoms have subsided. We hope this is over for you soon.
Staff Dentist
Comment –
Pain after 5 days
I am now into my 6th day following root canal treatment. I have suffered quite severe pain throughout. Most nights it wakes me up. I have tried not to take too many painkillers and I don’t want to rely on such. I have been taking 8/500 cocodamol and occasionally 30/500cocodamol . I was told by my dentist that it could take up to 2- 3 weeks for things to settle down. I have been brushing 4 – 5 times a day and mouth washing , but more than that I am not sure there is much I can do. Anecdotally I have heard that these things can take some time. Do you have any advice for me to help?
SMJ
Reply –
Your dentist most likely expected that as each day passed after your endodontic treatment the level of pain you experienced would continue to subside. What you’re experiencing seems beyond that, so without question you should report to them.
The medication you are taking, co-codamol, is a combination pharmaceutical containing paracetamol (referred to as tylenol in the USA) and codeine. Both of those compounds are pain relievers but neither has anti-inflamatory properties.
As discussed above on this page, the most common cause of post-root canal treatment pain is inflammation of the tissues that surround the treated tooth’s root. And because of that, pain relievers that also have an anti-inflammatory effect are typically more effective in controlling/resolving the patient’s post-op discomfort.
Ask your dentist about the possibility of including or switching to a medication that has anti-inflammatory properties (see NSAID discussion above).
Staff Dentist
Comment –
Query
Hello …. I also done first step of RCT yesterday,actually my tooth pains very badly from last 3 days ,Dr.tell me that there is a infection over the teeth and so much severe dental cavity … She clean the pulp and infectious area , and then place some medicine with cotton(it must be iodine)and then temporary filling cement which will be removed after some time or day . She tell me now tooth will not pain ….. But it’s still have pain even I can’t eat or place upper teeths on the RCT tooth even while doing brush i feel much pain … Will you please tell me when my pain will stop n I can eat properly ……
Amruta
Reply –
Your solution lies in contacting your dentist. Dentists expect patients to call if they are having problems.
There are a few more questions to be asked beyond what you tell us in your narrative, so we won’t speculate as to the precise cause or solution. But what you describe seems to lie within the realm of common complications, so handling your problem will probably be routine to your dentist.
Depending on the nature of the problem, in cases where immediate treatment from a person’s dentist isn’t possible (weekends, late hours), they may prescribe medications (antibiotics and/or pain relievers are a possibility) over the phone to the pharmacy so the patient can start with them and be comfortable until they can be seen.
Staff Dentist
Comment –
Swelling after root canal treatment
I had root canal treatment on LR4 in the afternoon two days ago. There was no swelling before the treatment. My jaw started to swell yesterday, chipmunk look, and has continued over night and seems worse today. Is this to be expected? The clinic is closed today, and I wonder if I need to go to A&E.
Marina
Reply –
Yes, it would be our interpretation of what you state that you need attention. The timing of the swelling suggests that there’s an active infection associated with your tooth.
You don’t state whether your tooth’s endodontic treatment was fully completed, or there is a second visit to come. Either way, what you’re experiencing is most likely just a temporary set back (as opposed to case failure). But each scenario would be handled differently by your dentist.
You state that your dentist’s office is closed. But don’t overlook that it’s common for a dental office to at least offer telephone support during off hours.
It’s common for the management of what we interpret as being your situation to include a regimen of oral antibiotics, and generally the sooner that’s started the better. So telephone contact with your dentist, and their calling a pharmacy, could get that going for you (if they think it’s needed). If some type of hands-on treatment could aid your situation too, they might offer to do that for you too.
In lieu of your dentist, yes, a visit to an emergency room would likely result in at least a prescription for antibiotics.
Staff Dentist
Comment –
Discomfort after completed root canal.
I had a root canal procedure completed like 3 months ago,after like a week i felt discomfort and sensitivity in the tooth and went back to the dentist who did an ex-ray and it showed that the filling had had gone beyond the tip of the tooth.He had to redo it again and it was completed like a month ago.All was well until a week ago when i felt discomfort and slight pain again.went back to the dentist and the x ray showed that all is well.the work was well done.what could be the problem?i had feeling this way.sometimes i feel like the left part of my mouth is numb but the pain is manageable but irritating
Ann K
Reply –
If you’ve read through our root canal complications/failure page, you’ll see that there’s a myriad problems that might exist, so it’s impossible for us to wager much of a guess.
In regard to x-ray evaluation, while it might be used to definitively diagnose a tooth’s condition, and while everything looking good on the x-ray is never a bad sign, the look of treatment on a film may not reveal all that is going on. For example, it may simply be too early for signs to have appeared.
What’s needed is for you to continue to monitor your tooth and stay in touch with your dentist about your status and changes you notice. You don’t mention if the dentist treating your tooth was a general dentist or endodontist. For difficult cases, evaluation by a specialist may be needed to diagnose what’s going on.
Staff Dentist
Comment –
Post root canal numbness.
I had a root canal 5 days ago. I am experiencing numbness on several of my adjacent teeth including my left front tooth. I called my dentist and he said it was infection From the treated tooth and prescribed antibiotics. He said I should notice the numbness subsiding within about 24 hours. So far no effect from the penicillin. What are your thoughts. Thank you.
Bill
Reply –
Normally it takes oral antibiotics about 24 hours to begin to have an effect. So there might be some question if your dentist was stating that fact or really expecting your condition to resolve by then.
You don’t say if the treated tooth was an upper or lower one. There is a postoperative complication termed paresthesia, which is much more likely to be a problem when a lower tooth has been treated. It’s associated with persistent numbness.
With root canal work, it could be a complication associated with the numbing injection, or the work itself. We don’t discuss this complication on our pages as it specifically relates to endodontic cases, but do cover it as a complication associated with tooth extractions (use the link).
Staff Dentist
