Intraoral sinus tracts – Dental fistulous tracts. | Recurring, persistent gum boils.
What is a sinus tract?
In dentistry, the term “sinus tract” refers to a situation where:
Pus coming from a chronic endodontic infection (a long-standing infection associated with the nerve space inside a tooth) …
… has established a drainage pathway that starts at a point in the area of the infected tooth’s root …
The anatomy of a sinus tract.
… that burrows through the jawbone (this small tunnel called a “sinus tract”) …
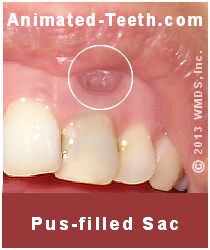
… to an exit terminus inside the person’s mouth. This opening takes the form of a persistent or recurring pimple-like lesion (“gum boil“). It’s usually located in a location immediately adjacent to the infected tooth.
▲ Section references – Hargreaves
Associated terminology.
The terms “fistulous tract” or “dental fistula” are sometimes used to refer to this type of lesion. However, according to formal medical terminology, their use is technically inappropriate. (Hargreaves)
Despite the word “sinus” being a part of the term, a person’s nasal sinuses typically have no involvement with the lesion and, in fact, this condition can be associated with either a maxillary (upper) or mandibular (lower) tooth.
What you need to know.
We’ve divided our coverage of this subject into the following topics:
- Signs and symptoms of having a sinus tract.
- How and why do sinus tracts form?
- Diagnosis.
- Treatment and healing.
Signs and symptoms of sinus tracts.
Here are the usual characteristics associated with a dental sinus tract.
a) There’s usually no tooth pain.
While the formation of a tract is a sign of a dental infection, the tooth in which it’s harbored typically remains asymptomatic (symptom-free). However, the tooth may have a history of producing pain and/or swelling at some point before the tract’s formation. (Hargreaves)
Why no discomfort?
Dental pain that’s caused by pus formation coming from an active tooth infection is due to the buildup of pressure that occurs. Once a sinus tract has formed, the infection’s pus has a way of venting off and therefore no pressure buildup occurs and no toothache is felt.
Due to the lack of pain, a tract may go unnoticed, possibly for years. Many times they’re only discovered through the thoroughness of a dentist’s routine clinical examination. (Tronstad)
Gum tenderness may be noticed.
The gum boil/pimple that forms at the tract’s terminus (opening in the mouth), and possibly the gum tissue that surrounds it, may show some tenderness. If so, it’s usually just slight. However, it may be noticeable enough to bring the presence of the lesion to the person’s attention.
▲ Section references – Tronstad
b) Gum boil location.
Proximity to the tooth.
A tract’s pimple-like terminus inside a person’s mouth frequently forms in a location that’s directly adjacent to the tooth that harbors the infection that has caused it.

That’s not always the case, however, and sometimes a tract empties at a point that’s some distance away. And since the problem tooth is frequently asymptomatic, determining exactly which of the patient’s teeth is at fault may not be immediately obvious to the dentist.
Making a diagnosis.
As a means of discovery, a dentist will often insert a slender rod of gutta-percha What’s this? directly into the tract and then take an X-ray.
The flexible nature of the gutta-percha (which is radiopaque, meaning it will show up on the X-ray) allows the cone to follow the tract’s path back to its source (the infected tooth), thus making the diagnosis obvious.
Location on the jawbone.
As illustrated in our diagram, the location of the gum boil that forms at the tract’s terminus usually approximates the level of the tip of the infected tooth’s root.
▲ Section references – Tronstad, Hargreaves
c) Gum boil size.
The size of the pimple-like lesion that forms at the tract’s orifice may increase and decrease (enlarge and deflate) over time. This fluctuation may occur over a daily, weekly, or even monthly time frame.
Compared to the picture above, the pimple is now fuller (retains some pus).
Why does this change take place?
The way the gum boil changes (inflates/deflates) is due to the amount of pus it tends to retain.
The overall quantity of pus that vents through the tract will wax and wane in step with the current level of activity of the tooth’s infection.
Once this volume of pus has reached the tract’s intraoral terminus, its ability to pass freely on through the gum tissue without being restricted or retained will influence the current size of the lesion.
An example.
If the tract’s orifice has become blocked or restricted (like the case where partial healing has occurred during a period of low infection activity), the pimple will inflate because some quantity of pus will be trapped or retained in its soft tissues.
Then, once the tract has opened back up (possibly due to the pressure resulting from pus accumulation), drainage can resume, thus bringing down the size of the pimple.
▲ Section references – Tronstad
d) Foul taste.
Since a sinus tract is simply a drain for pus, the discharge coming from one may have a noticeably bad taste. Sometimes this is a tip-off to a person that their lesion exists.
How and why do sinus tracts form?
The process.
Your body’s response to the presence of infection is a process termed inflammation. And some of the chemical mediators produced by this process trigger bone resorption (bone tissue breakdown). As a result, tract formation begins.
- This process tends to follow the path of least resistance, which is often also the shortest route possible. This explains why the tract’s opening inside your mouth frequently lies directly adjacent to the location of the infected tooth’s root tip(s).
- The direction the tract takes isn’t always so predictable. In some cases, it will confusingly terminate some distance from the tooth. It’s even possible for a tract to vent pus into a person’s maxillary sinuses (sinus cavity).
The infection that has triggered the tract’s formation is typically characterized as being a chronic (long-standing) one, with the tract developing over time. But tract formation is possible in conjunction with acute episodes too (sudden swelling flare-ups).
▲ Section references – Tronstad
Diagnosis.
Sinus tracts form in association with infected teeth. So, from a standpoint of diagnosis, the challenge is to identify which tooth harbors the infection.
Methods.
a) Directly investigating the path of the tract.
Above on this page, we mention how a dentist will sometimes insert a rod of rubbery material (called gutta-percha) directly into the opening of a fistulous tract. Due to its flexible nature, as it is pushed further and further, it will passively follow along inside the tract.
Since gutta-percha is a radiopaque material, when the dentist takes an X-ray, they’ll discover exactly which tooth the tract leads to. Diagnosis made.
b) Additional methods.
When direct investigation of the tract isn’t possible, dentists have a multitude of other ways they can search for and identify infected teeth. Just like they do when patients have problems (periapical abscesses, dental abscesses) but no tract has formed. Methods include:
Percussion testing – This simply means your dentist will tap on your teeth to see if doing so causes any sensitivity.
Thermal testing – This evaluation tests how your teeth do or don’t respond to hot and cold stimuli.
Pulp vitality testing – One method involves passing a weak electric current to individual teeth to see how they respond.
Taking additional radiographs – X-ray evaluation of infected teeth frequently shows changes in the bone tissue that surrounds them. A few traditional dental X-rays or even a Cone Beam CT scan might be included in the examination.
FYI: These pages provide more detailed information about the kinds of tests dentists perform.
1) Endodontic testing methods. Jump
2) Endodontic X-ray evaluation. Jump
What treatment is needed when a sinus tract forms?
The tooth’s infection must be resolved.
The treatment process that’s required when a sinus tract forms is removing the associated tooth’s infection. Towards this goal, there are only two options:
- Endodontic treatment – Root canal therapy treats the infected nerve space inside a tooth. Performing it will clear up the infection (and associated pus) that has caused the tooth’s sinus tract to form.
- Tooth extraction – If a decision is made not to perform endodontic therapy, the only other treatment option that exists is tooth extraction. (The tooth’s infection is cleared up by way of removing the tooth that harbors it.)
Healing.
Once the culprit infection has been resolved, the factors that triggered the tract’s formation are gone too. The tract and its surface lesion (gum boil) can be expected to close within a few days. Usually, no assistance from antibiotic therapy is needed. (Hargreaves)
Complications.
In cases where rapid healing does not occur, further evaluation is required. At this point, the assumption would be that either the tooth’s endodontic therapy was not successful in resolving the tooth’s infection or there are additional factors involved.
As an example of other possible causative factors, continued infection and pus formation could be due to the presence of periodontal disease (gum disease).
What’s next?
We have a lot more information about having root canal therapy.
Page references sources:
Hargreaves KM, et al. Cohen’s Pathway of the pulp. Chapter: Instruments, materials, and devices.
Tronstad L. Clinical Endodontics. Chapter: Reaction patterns.
All reference sources for topic Root Canals.
