What is root canal treatment (endodontic therapy)?
What does having root canal therapy do?
You may find yourself in a situation where you’ve been told that your tooth needs root canal treatment. And you understand that having it offers a way of saving your tooth.
What you don’t get, however, is how it accomplishes this. You don’t understand the underlying purpose of having endodontic therapy and what it changes about your tooth.
We answer these questions on this page. We outline the goals and objectives of this procedure and explain what’s different about your tooth afterward that makes it so it can be retained and rebuilt instead of having to be extracted.
What is root canal treatment?
Root canal therapy is a dental procedure dentists use to treat the interior of a tooth, the space that was originally occupied by its “nerve.” This procedure is also referred to as endodontic therapy.
Root canal therapy is used to treat conditions involving a tooth’s nerve space.
During treatment, the space is cleansed, disinfected, and sealed off.
Definitions.
The formal terminology for a tooth’s “nerve” is “pulp tissue.” However, for convenience and familiarity’s sake, on our pages, we use each of the following terms interchangeably:
Nerve = Nerve Tissue = Pulp Tissue = Dental Pulp
FYI: Collectively, the three videos found on this page provide a quick overview of the purpose of root canal treatment. Our most detailed information, however, is found in this page’s text.
Page highlights as a video –
Note: Dental-Picture-Show’s content and videos have now been absorbed into Animated-Teeth.com.
What is the purpose of root canal treatment? / What does it accomplish?
Dentists use root canal therapy to treat dental conditions that have compromised a tooth’s nerve tissue and associated nerve space. A dentist would refer to these kinds of conditions as endodontic pathology.
By performing treatment …
The dentist resolves the tooth’s nerve-space condition. (By way of removing dead or dying pulp tissue, sanitizing and disinfecting the tooth’s root canal system, clearing up bacterial infection, etc … And then filling in and sealing off this space.)
The completed treatment sets the stage so the tissues that surround the tooth’s root that have been irritated by its condition can heal and return back to a normal healthy state.
The root canal procedure is a two-stage process.
Endodontic therapy is usually thought of as a two-stage process. During the first stage, the interior of the tooth is cleaned out and disinfected. As a second step, this cleansed space is filled in and sealed.
Stage 1: Cleansing the tooth’s interior.
This first portion of the procedure involves removing remnants of the tooth’s pulp tissue from within its nerve space (pulp chamber and root canal system).
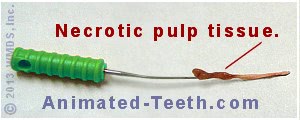
Nerve tissue that’s been removed from a tooth.
Depending on the nerve tissue’s current status, this may include live, inflamed, or necrotic pulp tissue. It also includes tissue breakdown byproducts that are a consequence of nerve degeneration.
Microorganisms (bacteria, fungi) that have invaded the tooth’s interior and the associated irritants, debris, and contaminants they have formed are removed too.
Stage 2: Sealing off the tooth’s interior.
Once the tooth’s interior has been cleaned and disinfected, its procedure is completed by filling in and sealing off this cleansed space. Doing so prevents contaminants and microorganisms from leaking back into or out of the tooth.
More details about the root canal procedure –
Stage 1: Cleaning the tooth. – What does this step accomplish?
Background.
Dentists use the same basic root canal procedure to resolve a wide range of nerve-related problems. For example, this fix is the required solution when a tooth’s pulp tissue is:
1) Irreversibly inflamed.
2) In the process of dying.
3) Completely necrotic (dead).
It’s also the solution that’s needed when the tooth’s interior harbors infection (either chronic or acute).
And even though each of these conditions is different, what they all have in common is that they each involve, or ultimately will at some point, a situation where the tooth’s nerve space harbors contaminants (typically related to infection) that will leak out of the tooth’s root tip and persistently irritate (inflame) the tissues that surround it. Common symptoms associated with this phenomenon are pain and swelling.
This step’s goal.
Therefore, as the underlying purpose of the cleaning portion of the root canal procedure The steps., the dentist’s goal is to sanitize the interior of the tooth as effectively as possible. So irritants won’t exist inside it to ultimately leak out and persistently irritate the tissues that surround its root.
In their attempt to accomplish this goal, they’ll remove the remaining remnants of the tooth’s pulp tissue (live or dead), the organic debris left over from the breakdown of this tissue, microorganisms (bacteria, fungi), and the toxins and other byproducts they have created.
Page highlights as a video –
Note: Dental-Picture-Show’s content and videos have now been absorbed into Animated-Teeth.com.
Stage 2: Sealing off the tooth’s interior. – What does this step accomplish?
During the sealing aspect of the root canal procedure The steps. the dentist will fill in and seal off the (now empty and disinfected) nerve space inside the tooth. They’ll need to use an inert biocompatible material. A rubbery compound called gutta-percha is usually chosen for this job.
Related to this step, there are two main goals that the dentist is trying to achieve.
- One of them is for the filling material to create a seal that prevents contaminants from seeping back into the tooth and recontaminating/reinfecting its interior space. (If this occurs, the tooth would again be a persistent leaking source of irritants to the surrounding tissues.)
- The other goal is just the opposite. The seal prevents any irritants still trapped within the tooth’s root canal system from seeping out (we explain in greater detail below). If this is not prevented, once again, the tooth would be a persistent source of irritants to the tissues that surround its root.
Sealing the root canal space (filling it in) prevents contaminants from entering or exiting it.
Following the completion of these two treatment stages, what has been gained?
What is the outcome of successful root canal treatment?
- With its procedure now complete, the tooth will no longer leak irritants into the tissues that surround its root and they can heal and return to normal. Once they have, they will remain healthy and symptom-free.
- Even though the tooth no longer contains any pulp tissue, once it has been properly rebuilt it will function and otherwise seem just like a normal live one. Its nerve will never be missed.
▲ Section references – Torabinejad
One last point.
How is it that contaminants can seep out of a treated tooth? Hasn’t its interior been cleansed?
Background.
This is a potential problem because a tooth’s root canal system doesn’t really have a precise shape like we show in most of our illustrations.
The tooth in the animation shown below is slightly more realistic. It illustrates that the canal inside a tooth’s root can be like a river, in the sense that it has a main channel that may give rise to small divisions that meander away and then return or else branch off and follow a different route entirely.
This poses a significant challenge for the dentist.
In an attempt to cleanse this type of convoluted anatomy (which must be assumed to exist to some extent with every tooth), a dentist will rely on a two-pronged approach when cleansing a tooth’s root canal system.
- Instrumentation – The dentist will use root canal files to scrape and clean Process explained. the walls of those aspects of the canal system they can fit into. (This will be the main/larger canals of the system.)
- Canal Irrigation – They’ll also rinse out the tooth’s interior Process explained. with a disinfecting solution, in hopes that it will seep into the smaller branches of the canal and cleanse them.
Even with instrumentation and irrigation, complex root canal systems can be impossible to completely disinfect.
But despite their best efforts, it’s always possible that some amount of debris will still remain. And in fact, the reality of the matter is that studies have shown that the root canal system of a tooth really can’t be completely cleaned and disinfected. (Hargreaves)
So, the sealing process ensures that these (hopefully minimal level of) contaminants that remain are entombed within the tooth and therefore can’t seep out and persistently irritate the tissues that surround its root.
▲ Section references – Hargreaves
Page highlights as a video –
Note: Dental-Picture-Show’s content and videos have now been absorbed into Animated-Teeth.com.
Why is the issue of contaminants harbored within a tooth such a big deal?
Because teeth are cavernous objects, your body’s ability to handle infections inside them is different than with other parts of your body.
A comparison –
A) What happens with soft-tissue infections.
Imagine that you have a cut on your finger and it has become infected. Immediately, your body will activate your immune system to mount a response.
White blood cells will be dispatched to the area through your lymphatic and blood vessels. These cells will fight the invading bacteria, and in most cases, they will win. They will destroy the harmful microorganisms and clear away any resulting debris.
B) What happens with infections inside teeth.
Once a tooth’s nerve tissue has started to degenerate (die-off) and bacteria have taken up residence inside the tooth’s nerve space, it’s difficult for white blood cells to effectively get at the microorganisms to combat them.
There’s limited transportation available.
Due to the deteriorated state of the tooth’s pulp tissue, the blood and lymphatic vessels inside the tooth that are used to transport these cells directly to where they are needed, either no longer exist or have been compromised.
That means the nerve space inside a tooth (especially when fully necrotic) can provide a nice cozy cave-like location for bacteria because it’s a place where your body’s defense mechanisms have a hard time getting at them and being effective. (Ingle)
The empty, hollow space inside a necrotic tooth is a difficult location for your body’s immune system to fight infection.
The consequences.
At best, your body will only be able to cordon off the infection. Since white cells can’t get inside the tooth to effectively combat the bacteria there, your body will set up a perimeter of defensive tissue and cells around your tooth’s root to contain the infection.
As a worst-case scenario, the infection may massively overwhelm your body’s wall of defense and cause an acute tooth abscess, resulting in pain and swelling.
What actually happens is often a mixture of both. One where the tooth’s infection remains quiet (cordoned off and controlled) most of the time, with periods of (hopefully minor) flare-ups where some level of tenderness, pain, or swelling is noticed.
So, bottom line, here’s what root canal treatment accomplishes.
As opposed to the example above, performing endodontic therapy provides an outcome where the infection associated with a tooth can be cleared up by your body’s normal defense mechanisms.
- The root canal treatment assists your body’s infection-fighting abilities by removing (disinfecting) and sealing off (entombing) bacteria and contaminants inside your tooth that it would otherwise have difficulty dispensing with.
- Following the completion of your tooth’s treatment, no further leakage of irritants from its root should occur.
- Any microorganisms and contaminants that have already exited and inflamed the tissues that surround your tooth’s root can be dealt with in a normal fashion by your body’s immune system.
- The expectation is that this cleanup and healing process will be successful. The result will be an inert tooth root (one that doesn’t leak irritants) surrounded by normal, healthy, symptom-free tissues.
▲ Section references – Hargreaves
Additional details you need to know to understand root canal treatment.
Where precisely in a tooth is its nerve?
Teeth are not solid. Instead, inside every tooth lies a hollow space filled with the tooth’s pulp tissue (“nerve”). Dentists use the following terms to refer to various portions of this nerve space:
a) The pulp chamber.
This is a cavern that lies pretty much in the center of a tooth’s crown (the portion that is visible above the gum line).
Total tooth nerve space = Canal(s) + Pulp chamber
b) Root canals.
Root canals are tiny tunnels that run the length of a tooth’s root. (From its pulp chamber down to the root’s apex (tip).)
(FYI: Measuring the length of these canals How it’s done. is a very important part of the root canal process.)
As a rule, every tooth root (note: some teeth have more than one root) will contain at least one canal. But a root having more than just one canal is possible, and commonplace with some specific kinds of teeth.
(For more in-depth information, visit our page: How many roots and root canals do teeth have? What’s normal? | Variations.)
Isn’t it important for a tooth to have a nerve?
No, not really. A tooth’s pulp tissue plays a role in its formation and development. But once that’s been completed, it’s not so vitally important. So, having it removed during root canal treatment isn’t that big of a deal.
You don’t really get much “feeling” input from a tooth’s nerve.
Under normal circumstances, the nerve tissue inside our teeth provides us with comparatively little information.
Yes, when subjected to pressure or temperature extremes, or exposed to severe insult (like advancing tooth decay or the formation of a crack), teeth do respond with a painful sensation. But other than that, the nerves inside our teeth remain relatively unresponsive.
Proprioception.
You might think that when you push on your teeth, or else close them together, the pressure sensation that you feel (proprioception) is a signal from within your tooth.
Actually, most of this sensation (around 70%) comes from the nerve fibers found in the tissues that surround your tooth’s root, with the remainder originating from its pulp tissue (Eliyas). On a practical level, however, this loss is not usually noticed.
You’ll never miss your tooth’s nerve.
Due to the above, from a standpoint of normal function, the presence of live nerve tissue within a tooth is pretty much optional. If it’s present and healthy, then wonderful. But if it’s been removed as a part of root canal treatment, then that’s fine too. You’ll never miss it.
For more information about having root canal …
Here’s a listing of additional pages we offer that further describe aspects of having endodontic therapy.
- What you can expect during your procedure The steps. What they’re like., as well as afterward. The post-op experience.
- Ways teeth are rebuilt What decides? following their treatment including: Crowns Post & cores
- Treatment costs. Endodontic fees.
- Why a tooth’s therapy might fail. Reasons.
- Treatment alternatives Options (such as implants vs. root canal Which is better?).
Page references sources:
Eliyas S, et al. Restoration of the root canal treated tooth.
Hargreaves KM, et al. Cohen’s Pathway of the pulp. Chapter: The core science of endodontics.
Ingle JI, et al. Ingle’s Endodontics. Chapter: Irrigants and intracanal medicaments.
Torabinejad M, et al. Endodontics. Principles and Practice. Chapter: Endodontic microbiology.
All reference sources for topic Root Canals.
