Rebuilding your tooth after its root canal treatment.
Every root-canalled tooth will need a final restoration.
After a tooth’s endodontic therapy has been completed it will require some type of permanent or “final” dental restoration to return it to its previous shape and function.
This page discusses the different options you have in deciding how your tooth is rebuilt (primarily either a crown or filling). And details what factors need to be considered when choosing between them.
Topics this page covers:
- Important factors in choosing between a filling and a dental crown (based on the needs of your tooth).
- General guidelines about which makes the best choice.
- Fillings vs. crowns – What does dental research say about the benefits of crown placement?
- How soon does your tooth’s final restoration need to be placed?
FYI: You may also be interested in these associated pages about rebuilding root-canalled teeth:
- Can a tooth’s original crown be reused? When?
- Will a post and core What’s this? be required?
A crown or filling after a root canal, which makes the better plan?
For the most part, the two basic options that you have as final restorations for root-canalled (root-filled) teeth are placing a dental crown or else a filling.
What’s the difference?
These two kinds of restorations are quite different in both their construction and the purposes they are able to serve. In very basic terms:
Fillings.
Just like the name suggests, a filling primarily just fills in voids in a tooth. It replaces any missing portions.
Placing a filling will seal a damaged tooth back up and restore it to its original contours. The appearance of the tooth is often improved too. But that’s about all. Fillings are kind of like dental patchwork.
FYI: You may see dental fillings referred to as intra-coronal restorations or else direct restorations.
Dental crowns.
Compared to a filling, a crown is typically considered a more robust and lasting type of restoration due to the types of materials it’s made of and the way it fully encases a tooth and its cusps.
Placing one creates an excellent seal for a tooth (prevents bacterial leakage into the tooth’s interior). Some types of crowns provide a substantial strengthening effect (fracture resistance). And as a side benefit of our purposes here, placing one gives a dentist full control in remaking a tooth’s appearance.
FYI: You may see dental crowns referred to as extra-coronal restorations or else indirect restorations.
Then what’s the catch? Why isn’t a dental crown placed on every tooth that’s had a root canal?
The nature of each type of restoration is different.
A big difference between placing a filling versus a crown is that making a crown is a fairly aggressive process. When making one for a tooth a significant amount of its remaining tooth structure is trimmed away. (On the order of 2 mm (1/16 inch) on all sides.)
That’s not really ideal, in the sense that a primary goal of dentistry and practitioners in general is to preserve natural tooth structure whenever possible. So if placing a filling can suffice, then that option makes the more appropriate choice because less healthy tooth structure is lost.
Cost differences.
Another primary consideration that frequently comes into play when deciding between the two is the treatment’s expense. The cost of a filling is less than that for a dental crown, usually by a wide margin.
So, if a filling makes a suitable choice as a final restoration for a root-filled tooth then that probably makes the better plan. If not, a crown should be placed.
So, how do you and your dentist decide when a filling might work out?
That’s pretty much the subject of the remainder of this page. So, let’s get started …
Important factors in choosing the right kind of final dental restoration for a tooth that has had endodontic therapy.
1) Does your tooth require strengthening?
Teeth that have had root canal therapy can be fragile, possibly significantly so. And if that’s the case with your tooth, placing a dental crown probably makes the better and safer choice.
Here are some common reasons why a root-canalled tooth may require strengthening:
a) Weakening as a result of having had endodontic treatment.
When performing root canal therapy, a dentist must create an opening Access cavity. in the tooth through which they will perform their work. However, making this hole tends to weaken the structural integrity of a tooth.
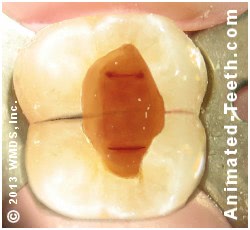
The access cavity created during the root canal procedure tends to weaken the tooth.
- Research suggests that when a conservative (comparatively smaller) opening can be made in a virgin tooth (one that did not have a previous dental restoration), the reduction in tooth stiffness that results (loss of strength) may be as little as 5% or so. (Eliyas)
- However, with many cases, like when the tooth’s individual root canals have been difficult to locate, the dentist may need to remove a comparatively greater amount of tooth structure, especially internally, to the point where the tooth may become significantly hollowed out.
b) Previous tooth damage that has occurred.
Teeth that end up requiring root canal treatment frequently have already experienced some type of major tooth damage. And as a result, have already been structurally compromised.

This tooth is very hollowed out and should have a dental crown placed.
- The tooth might have experienced trauma that has led to crack formation or outright fracture. The loss of tooth structure due to advanced tooth decay can significantly weaken a tooth.
- Research has determined that placing a filling on the chewing surface of a posterior tooth (like a molar) tends to reduce its stiffness (strength) on the order of 20%.
Larger-sized fillings, like those that touch neighboring teeth, have been found to result in an over 60% reduction. (Eliyas)
c) Changes in tooth dentin characteristics following a root canal.
It’s suggested that the chemical agents and medications frequently used during the cleaning phase of root canal therapy tend to decrease the flexural strength of dentin (the hard, calcified tissue that makes up the bulk of a tooth). Due to this effect, a treated tooth may be more prone to breakage. (Eliyas)
Does your root-canalled tooth require strengthening?
Clearly, only your dentist’s evaluation can make this decision. And you’ll just have to take their word for it. But due to all of the factors just discussed, don’t be surprised that by the time your tooth’s root canal treatment has been completed it may be at substantial risk for fracture, even when exposed to normal chewing forces.
If so, your dentist will most likely recommend that a crown should be placed rather than a filling. That’s because certain types of dental crowns can provide a strengthening effect How? for a tooth and therefore protect it.
2) All treated teeth will require a final restoration that creates a proper seal.
If saliva, and all of the bacteria, irritants, and assorted debris it contains, finds a way to seep past your tooth’s dental restoration, it will ultimately contaminate your tooth’s treated root canal system. (A phenomenon termed Coronal Leakage More details.) And as a result, its (previously successful) endodontic treatment will fail.
If contaminants re-enter a tooth, its completed treatment will fail.
That means, for long-term treatment success, the final restoration that’s placed following your tooth’s root canal procedure must be able to create a substantial and lasting barrier that prevents this phenomenon from occurring.
What determines if a restoration’s seal will last?
Times when a filling may suffice.
If the access cavity made in your tooth during its endodontic work (the opening through which your procedure was performed) was just minimal in size (small in comparison to the size of your tooth) and in a location that doesn’t get much wear and tear (like the backside of front teeth), a filling may be able to provide a suitable, lasting seal.
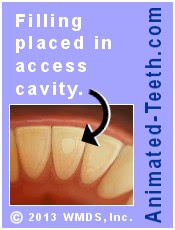
Conservative access openings in front teeth may only require filling placement.
With larger fillings, especially on posterior teeth like molars, the fear would be that the normal wear and tear that the restoration will naturally be subject to is much more likely to result in significant deterioration and breakdown (either gradually or suddenly). To the point where the process of coronal leakage could likely occur.
Dental crowns typically create an excellent seal.
Dental crowns, due to the way they cup over and encase a tooth, have a reputation for creating a very substantial and lasting coronal seal. For this reason, your dentist may feel that this option makes the more predictable type of final restoration for your case.
3) Final restoration longevity and durability are important factors.
The kind of permanent restoration chosen for an endodontically treated tooth must be one that your dentist feels is durable and can provide lasting service. This is important in both maintaining the structural integrity of your tooth and maintaining the seal that it creates for your root canal work.
a) Comparing the longevity of fillings vs. dental crowns.
Crowns.
Crowns are generally considered to be the most durable and longest-lasting type of dental restoration. Research studies show that it’s routine for a crown to provide service for 10 years and longer. (The type of crown that’s placed can be a factor.)
Fillings.
The lifespan of a dental filling is typically expected to be shorter than a crown but the size of the restoration and the type of dental restorative it is made out of (composite resin [white fillings] vs. dental amalgam [silver fillings]) are significant variables.
Small fillings, especially those that aren’t regularly and directly exposed to chewing forces, can last significantly beyond what’s typical.
b) Example cases for filling and crowns.
a) For relatively intact teeth.
It’s possible that a tooth that …
- Just has a conservative access cavity …
- And no other history of significant tooth structure loss (such as a previous cavity, filling, or breakage)
… might be successfully restored with just the placement of a dental filling.
This approach may be best suited for front teeth (incisors and canines) where the direction of force applied is typically non-axial.
With back teeth (premolars and especially molars), forces are more commonly directed straight down (axially). And for this reason, placing a restoration that creates a reinforcement effect (like a crown) may make the more prudent choice.
▲ Section references – Eliyas
b) More compromised teeth.
In comparison to teeth that are still in relatively pristine condition, those with large fillings or extensive decay, or teeth that fractured prior to their receiving root canal treatment, are probably best restored with a dental crown.
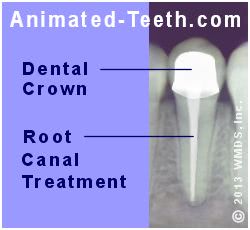
X-ray showing a tooth’s completed treatment and dental crown.
(In cases where a large amount of the tooth’s natural tooth structure is missing, a dental post and core may be required before crown placement. Why?)
This approach may be needed for either front or back teeth, simply depending on how broken down they are. Crown placement is especially appropriate for deteriorated molars, a type of tooth that must be able to withstand heavy chewing forces.
What type of final restoration makes the right choice for your tooth?
General guidelines.
- Placing a dental crown has increasingly become the “standard of care” that’s considered appropriate for endodontically treated molars. (See statistics section below.)
- For other teeth, especially relatively intact front ones (incisors and canines), and even possibly premolar teeth, the decision to place a dental filling may make a perfectly appropriate choice.
When a filling is considered …
The decision here is basically one of judging if the requirement for sealing the access cavity (to protect the integrity of the tooth’s root canal work) can be met by a filling, especially over the long term where restoration strength, durability, and longevity will all be factors.
FYI: In comparison, a crown is generally considered to provide an excellent seal and more predictable and lasting service.
Additionally, the filling (its size and shape) must also be an appropriate choice for the tooth in terms of not leaving it at significant risk for catastrophic failure (i.e. tooth fracture).
FYI: This kind of risk is significantly minimized by crown placement.
Additional considerations.
Generally speaking, the advantages of placing a filling instead of a crown are that it …
- Avoids the aggressive tooth trimming that placing a crown requires. (There’s nothing positive about grinding down a tooth if it doesn’t need the benefits that a crown can provide.)
- A filling can be placed at less expense than a crown.
- It takes less treatment time and usually fewer appointments to place a filling.
How to decide.
The decision between the two typically boils down to these points:
- The extent of original tooth structure that remains. – Is the tooth still structurally intact? Or does it need significant rebuilding and strengthening?
- The degree of wear and tear and level of force the restoration (and tooth) is expected to be subjected to. – Can a filling be expected to provide predictable lasting service? (Small ones typically can. With many larger ones, there would be a question.)
Obviously, your decision will almost always be based on the advice of your dentist. But it’s these types of issues and factors that they should have considered, and be able to provide an explanation to you about. There is no cookie-cutter best choice that applies to all cases.
Dental research confirms the benefit of a dental crown when one is indicated.
Several studies have evaluated the outcomes of teeth that have had endodontic therapy and then were, or were not, crowned. Here are the findings of some of those studies.
1) Aquilino (2002) – This study evaluated the track record of 400 endodontically treated teeth and found that those that were not crowned were lost at a rate 6 times greater than teeth that had dental crowns placed.
2) Nagasiri (2004) – This study evaluated 220 molars that did not receive dental crowns after root canal treatment. The survival rates of these teeth at 1, 2, and 5 years were 96%, 88%, and 36% respectively.
3) Lynch (2004) – This study evaluated 176 teeth for a three-year period following the completion of their endodontic treatment. The following survival rates were observed for teeth with the following types of restorations: cast restoration (dental crown) – 92%, amalgam restorations (“silver” filling) – 67%, composite restorations (tooth bonding) – 35%.
▲ Section references – Aquilino, Nagasiri, Lynch
How soon does the permanent restoration need to be placed?
Your dentist will make a recommendation about the time frame that is appropriate for placing your tooth’s final restoration (dental crown or filling).
The phrase “as soon as is reasonably convenient” (meaning not an emergency but definitely a priority), often applies to this situation.
Why the rush?
In general, the temporary restoration that has been placed is just that. Here’s why:
Risk factors.
- A temporary can’t be relied upon to provide adequate protection or strengthening effect for the tooth over longer periods, thus leaving it at risk for breakage or fracture.
- When compared to a permanent restoration, the seal that a temporary creates isn’t as lasting, thus placing the tooth at risk for recontamination.
- Temporary restorations frequently don’t meet the same high standards as permanent ones. This can make brushing and flossing around them difficult and ineffectual.
FYI: Our root canal aftercare page Jump explains these risk factors in greater detail.
What’s next?
There’s a lot more to learn about rebuilding teeth after completing theirt root canal treatment.
Page references sources:
Aquilino S, et al. Relationship between crown placement and the survival of endodontically treated teeth.
Eliyas S, et al. Restoration of the root canal treated tooth.
Lynch C, et al. The influence of coronal restoration type on the survival of endodontically treated teeth.
Nagasiri R, et al. Long-term survival of endodontically treated molars without crown coverage: A restrospective cohort study.
All reference sources for topic Root Canals.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Is crown necessary?
My tooth that’s just had root canal had a filling in it for years and it did just fine. My dentist said we should now place a crown. Is that really necessary? It’s a big added expense. I’d rather have another filling placed.
Heather
Reply –
We’re not going to have enough information about your tooth and situation to know what’s needed. Your dentist is in a position to have an idea, and evidently they think that crown placement makes the best plan.
There are two important factors that you should keep in mind:
1) The restoration that’s placed needs to be able to create a seal that prevents bacteria and such from seeping back into the interior of your tooth (see coronal leakage link above). Crowns are very good at preventing this.
2) Your tooth probably isn’t as strong and fracture resistant as it was previously. (For example, it’s been substantially hollowed out during your root canal treatment.)
It’s not so much that a filling can’t provide a seal and serve as a strong restoration, it’s just that crowns do this so much more reliably and predictably. Evidence of this is found in the studies mentioned above. Teeth that have had crowns placed after their root canal treatment tend to have a higher survival rate.
That doesn’t mean that all teeth require a crown. It in part depends on how much tooth structure has been lost. In your case, we’re assuming that the filling that existed previously was somewhat sizable (a repair large or involved enough that root canal treatment was ultimately needed).
If instead the hole in the tooth is just a small one (and really only your dentist would be able to make this judgment), a filling might suffice just fine.
Ideally the crown (or whatever permanent restoration is chosen) would be placed promptly after the completion of your tooth’s endodontic work. If finances or such make that difficult, bring the issue up with your dentist and see if they can offer any solutions/alternative plans (payment plan, placing the crown as soon as your next insurance cycle allows, etc…). Good luck.
Staff Dentist
Comment –
Composite filling in root-canalled tooth one year before crown?
I need to have a root canal in a molar tooth, since there is a cavity under the old silver filling on the chewing surface. From two other root-canalled molars I know the tooth needs a crown and that it takes some time for the lab to create the crown. But I don’t have the time waiting for that, as I am expatriated to Asia very soon. Therefore I will ask my dentist to prepare a regular composite filling in my root-canalled molar tooth, hoping that such a filling will last a year or so (as a temporary one-year solution), then I will have the crown once I return from Asia. Is that a suitable solution for a root-canalled molar? Don’t know if one year is too long to wait for a crown on a weakened root-canalled molar tooth even though it has a composite filling or whether it will break during that year. Alternative is to get a crown while I am in Asia
Flemming
Reply –
In regard to the timing of the crown placement, we’ll defer to your dentist’s opinion. There is no question that a 1 year delay in placing the crown isn’t usually ideal. But for some teeth (possibly even a molar) some type of conventional filling might provide an adequate final restoration. Just ask your dentist what they would do for their own tooth (wait until you return, or have the crown placed in Asia).
In regard to making a go of a dental filling. The quality of the coronal seal of the restoration can be improved by the dentist extending the filling down into the opening of each of the canals just a few millimeters.
(Here’s a link to a paper that discusses exactly that, and mentions that dental composite creates the superior seal as compared to other restorative materials. But also mentions that all groups showed some leakage, so that might be your answer right there.
An assessment of coronal leakage of permanent filling materials in endodontically treated teeth: An in vitro study.)
In regard to filling placement and protecting a potentially fragile tooth, your dentist would probably make the occlusion on the tooth as passive as possible (meaning it doesn’t get much pressure when you bite down or slide your teeth around when touching). And then of course, you would want to favor the tooth as much as possible.
While it would mean utilizing a different dentist, same-day crown placement is a possibility in some dental offices. Probably the most durable type of crown they would have to offer is (monolithic) IPS e.max. You might ask your dentist about suggestions with this option.
And finally, if you’ll Google “best dental schools in the world” (and consider that a proxy for the type of dentistry practiced in that country), several seem to be in Asia.
Staff Dentist
Reply –
Thanks a lot for a very informative and detailed answer. I had my root canal done yesterday. My dentist was clearly in his opinion that I should have the crown very soon and that 1 year delay is far too long. But he accepted my wish and made a composite filling (don’t know if he extended it down the canals as you mention). But he shaped the tooth/filling so it will not have the hard pressure for chewing and of course I will try to favor the tooth as well. He also mentioned that dentists should be quite good in Asia, so maybe I should consider have the crown while staying there.
Flemming
Comment –
Restoration After Root Canal
I had a root canal performed on my #2 molar. I would be OK with only a filling as the tooth is not visible and the repair would be less expensive than a crown.
RamondJ
Reply –
The issue isn’t about appearance. Instead it’s (always) about how well the restoration seals the tooth (so to prevent coronal leakage) and possibly a restoration is needed that can strengthen your tooth.
If you haven’t already, you should read this page about final restorations for root-canalled teeth. (Make sure to read the statistics section.)
Possibly just placing a filling is satisfactory for your situation. But only your dentist can advise you on this issue.
Staff Dentist
Comment –
Very informative.
Hi, thank you for the great site, it’s very informative!
I had a root canal done for my upper first molar 12 years ago. I remember the dentist at the time mentioning that the tooth might become brittle over time and break at some point but no crown placement was offered. Since then I’ve seen a number of different dentists and while they have remarked that the root canal is quite extensive, no-one has suggested getting a crown, this includes an endodontist that I saw for an unrelated issue earlier this year.
However, reading information on your site and other sources it seems that crowns are the current standard of care for root canal aftercare. So should I be getting one? Does the fact that the tooth has been OK for the last 12 years means it’s a good sign and a prediction that it might last or has the tooth been getting brittler and I am at ever greater risk of splitting it as the time passes?
I’m a bit worried about getting a crown because it comes with its own fair share of possible complications and difficulties. Also it seems that with a crown it is not recommended to eat hard food such as nuts and popcorn and I imagine those would be the likely culprits for why a root canal tooth with a filling might break too. If so, could I just stop eating hard food now and not get the crown? Even now I consciously chew nuts and seeds with my wisdom teeth (of which I have all 4), to take the pressure off of the first molars, is that a good thing to do?
Thank you so much!
Toothy
Reply –
A dentist not suggesting work vs. you specifically asking them about the need for treatment really are two different things. So if you haven’t recently, you should bring up the subject with yours, pretty much the way you have here and let them advise you.
Here’s an article titled: Are full cast crowns mandatory after endodontic treatment in posterior teeth?. It seems to take the same general stance on issues as we’ve discussed them here on this page but provides greater detail.
You’ll note there is a section that addresses the issue of tooth structure changes after endodontic treatment.
And it mentions how the size/extent of the filling in the tooth significantly affects the tooth’s strength, and therefore whether or not a crown should be placed. (Here’s our similar page: Choosing between a crown and filling.)
You’re right that there can be possible complications with crowning a tooth. So one should only be placed for good reason. But if placed, the type should be one where concerns about breakage are non-existant or minimal.
The linked article above discusses “full cast crowns,” meaning all-metal ones. But there are other, more aesthetic appropriate crown options for molars too (scroll down on that page just a bit).
Forces directed to teeth can cause cumulative effects. Generally, small initial cracks can grow in size due to continued exposure to heavy forces. So, in regard to your root-canalled tooth and/or its neighbors, you should keep that in mind.
Like stated initially, you should bring up this issue with your dentist, the person that can evaluate your specific situation, so they can advise you one way or the other. Good luck.
Staff Dentist
Comment –
Crown question.
5 years ago I had a root canal done on canine #11. It died because my or orthodontist turned it too quickly. My dentist at the time placed a post in the tooth but never mentioned needing a crown. This year I went to a new dentist who recommended getting a crown done as the post is exposed on the back of the tooth. SHould you crown a front canine that from the outside looks okay? Thank you
HR
Reply –
Your question is hard to answer because it depends on how much of the tooth is original tooth structure vs. dental materials.
It’s usually considered that a post is only required if it is needed to help anchor the dental materials that are used to rebuild the tooth. (Our post and cores page explains.)
So if a large portion of your tooth was missing after the completion of the root canal work (possibly just on the backside), it would be expected that post placement was indicated. And it’s very common that related to the substantial rebuild job needed that crown placement often makes the preferred way to rebuild a tooth.
Following that scenario, that fact that your post is now exposed implies that the filling material originally placed has deteriorated (or at least substantially worn down) in just a few years. If so, a crown typically provides a more lasting, better sealing, restoration and probably therefore is indicated.
One can’t help but to notice that you state that your tooth required root canal treatment related to orthodontic trauma (as opposed to structural damage caused by advanced decay or tooth fracture).
It’s sometimes possible that with this situation (structurally pristine front teeth) the access cavity made can be quite conservative, and following the root canal procedure just placing a filling suffices. (A post isn’t needed because the filling needs no aid in retention.)
So consider the situation where just placing a filling can be considered an adequate final restoration for the root canal work, and (for whatever reasons) a post just happens to have been placed. And now the post is exposed.
Is it exposed because it wasn’t trimmed short enough originally and had just a thin layer filling material over it that has since worn down? With a possible solution being trimming the post shorter so a more adequate thickness of restorative can cover it?
So as you can see, only a dentist who has seen your tooth can answer these questions and make an appropriate treatment recommendation. So just ask again. But as they explain your situation, it would be expected that the issues described above might be mentioned.
It should be pointed out that, at least in theory, the exposed post places you at risk for the complication of coronal leakage, so you need to pursue a remedy of some fashion in a timely manner.
Staff Dentist
Comment –
Do we need both filling & a crown after Root canal?
I was suggested that after Root canal, filling will be applied immediately and after few weeks a crown needs to be added.
So my understanding is, you need to do Root canal first, filling next & optionally decide to have a crown.
or is it possible that we just do Root canal & crown directly without doing a filling?
SJ
Reply –
If you know that you do want a crown placed on the tooth, there’s usually no requirement for a separate filling step. The access cavity does need to be filled in and sealed off with some type of permanent material (ranging from dental cement to some type of filling material, depending on the preference of the dentist).
But whether doing that (often quick and simple) step should just be included in the cost of the crown could be debated. (Here’s an article that somewhat discusses that point. Generally, it would be considered that “core placement” (extensively rebuilding the tooth) would be a more involved procedure (and therefore a more justifiable fee) than just placing a filling.)
After quizzing your dentist some more, they may offer some additional information that makes it obvious why doing things the way you state is needed. But for most cases, that way (root canal, filling, wait a few weeks, crown procedure) certainly isn’t a requirement.
Staff Dentist
Comment –
Do I need a crown?
My front tooth with pulp necrosis had a root canal last week and the dentist just completed the treatment with a filling yesterday. As I see now, the tooth is totally fine; but it’s a little bit discolored compared to other teeth. Should I need a crown in this case?
JN
Reply –
Crowns are preferably placed for reasons other than just making a color change. A prime example is when the tooth needs strengthening, like discussed above.
When placing a crown isn’t the ideal solution, there are still ways to lighten a tooth:
1) Teeth bleaching treatments. – There are methods where the bleaching agent is applied externally or even inside the tooth. Both methods have pros and cons. Only your dentist could help you decide what’s the right choice for your tooth.
2) Placing a veneer. – With this method, the end result is one where the tooth’s color is changed as if a crown had been placed. It’s just that this is a less aggressive procedure (less tooth trimming) and therefore more favorable for your tooth.
Staff Dentist