Performing root canal on teeth that already have a crown.
Performing root canal treatment for crowned teeth.
Root canal therapy is sometimes needed for teeth that have already had a permanent dental crown placed on them. In fact, this is a fairly common situation. And in these cases, the question then becomes …
… What happens to the crown when the tooth’s root canal treatment is performed?
a) When a tooth already has a crown, the possible treatment options are:
- Removing the crown before its endodontic treatment is performed. (If that’s possible.)
- Or else, performing the tooth’s root canal procedure through an opening drilled through the crown. (The procedure’s “access cavity” is made through the restoration.)
b) What needs to be considered next?
In either case, after the tooth’s work has been completed, the dentist must determine if it seems reasonable to reuse the crown or if it must be replaced.
Table of contents –- Options when performing root canal therapy for teeth that already have a dental crown.
- Evaluating your crown for reuse following its root canal treatment.
- 1) Crowns that had an access cavity made through them.
- Is the crown still strong enough? – Metal vs. PFM vs. Ceramic crowns.
- Can the crown maintain an adequate seal? – Coronal leakage/Root canal failure.
- Advantages of crown replacement.
- 2) Reusing crowns removed before the tooth’s treatment. – Issues.
- Other ways to learn.
- This page’s highlights as a video.
- 1) Crowns that had an access cavity made through them.
- Is the crown still strong enough? – Metal vs. PFM vs. Ceramic crowns.
- Can the crown maintain an adequate seal? – Coronal leakage/Root canal failure.
- Advantages of crown replacement.
- 2) Reusing crowns removed before the tooth’s treatment. – Issues.
- This page’s highlights as a video.
This page’s highlights as a video –
Subscribe to our YouTube channel.
Ways a tooth’s existing crown can be managed during its root canal procedure.
In our coverage of root canal therapy The procedure., we explain how one of the first steps the dentist takes is creating an access cavity in the tooth. How? | Where? This is the opening through which they’ll then perform the tooth’s root canal work.
An “access cavity” provides entry into a tooth’s nerve space (pulp chamber + canals).
In the case where the tooth already has a dental crown, one of the following two scenarios will need to take place:
Option #1 – The dentist will remove the crown before making the access cavity.
When possible, this makes the ideal scenario. That’s because:
Making the access cavity shouldn’t affect the fit of the crown.
The portions of a tooth that are trimmed away to make an access cavity are usually unrelated to those that affect a crown’s fit and seal. (Primary concerns for these factors are the tooth’s height inside the crown and how the edges of the crown fit against the tooth.)
So, following the tooth’s work, the crown can simply be recemented back into place. All of the duties it provided for the tooth prior to its work can still be fulfilled. And with this scenario, the expectation would be that the outlook for the success of the tooth’s root canal work and the overall structural integrity of the tooth (and crown) would be ideal.
Why this scenario may not be possible.
Unfortunately, as simple as this plan sounds, the reality of removing a crown from its underlying tooth can be quite difficult (or even impossible) to do without damaging it or the tooth (discussed in more detail below).
So in most cases, a dentist will make an attempt at removal but will quickly move on to Option #2 if it doesn’t seem to want to come off relatively easily.
Option #2 – The access cavity will be made through the existing crown.
If the dentist determines that the crown won’t come off (or at least not easily or predictably), then they’ll have to drill the hole (access cavity) right through it to perform the tooth’s endodontic procedure (see picture below).
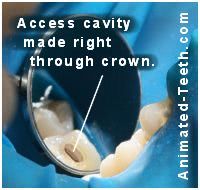
A dental crown with an access cavity drilled through it.
If a hole is drilled, what’s the outcome for the crown?
If this option is chosen a question then arises. Has making the access cavity through the crown compromised it, or the way it can protect the tooth and its root canal work? Can it still be used afterward, or will need to be replaced?
These questions are the subject of the remainder of this page. And as you’ll discover, the answer is typically:
- It may be possible to reuse the crown.
- But it’s probably a better plan to go ahead and replace it.
Discussed below are the types of factors that must be considered when deciding between these two options.
Evaluating your dental crown for reuse after root canal treatment.
Crowns that have had an access cavity made through them. – Issues and concerns.
1) Is the crown still strong enough to protect its tooth?
If the structural integrity (strength) of the existing crown has been compromised by the act of drilling a hole through it to make the access cavity, and therefore it can no longer be relied upon to protect the tooth (strengthen it, prevent tooth or root fracture), it will need to be replaced.

Drilling an access cavity through an all-ceramic crown will likely weaken it.
Issues that must be considered.
In practice, the degree to which a crown has been weakened by making a hole in it will vary. Here are some of the factors involved:
a) The type of crown.
There are different types of crown construction Kinds of crowns., and the strength characteristics of each kind will be affected differently when a hole has been drilled through it.
1) All-metal crowns.
Drilling a hole through an all-metal crown (like a gold crown) probably won’t significantly affect its overall strength and the level of protection it provides for its tooth. The same would go for crowns that have a porcelain covering on their side that shows (so the crown looks like a natural tooth) but their backside or chewing surface is all-metal.
2) Porcelain-fused-to-metal crowns.
Creating an access cavity through a PFM restoration probably won’t significantly affect its overall strength characteristics either.
But doing so may affect the integrity of its porcelain covering (outer shell), possibly resulting in chipping or fracture, especially in the region immediately around the access cavity. (This chipping effect could compromise the integrity of the restoration placed as a repair for the hole, see “filling placement” below.)
More extensive porcelain fracture is possible too. In many cases, this may only be a minor cosmetic concern. But if the loss is large enough, it may create a problem with both appearance and function.
3) All-ceramic crowns.
In comparison to types of crowns that contain metal, the process of creating an access cavity through an all-ceramic (“porcelain”) one presents the least predictable outcome.
Concerns about restoration strength and/or damage (such as microcrack formation) that may ultimately lead to failure are valid issues.
- Just as with PFM crowns, ceramic chipping immediately around the access cavity itself is commonplace.
(A study by Wood found edge chipping in 100% of ceramic crowns evaluated.)
- Beyond that issue, the remaining strength characteristics of the perforated ceramic restoration will need to be considered suspect too.
Logically, the amount of structural integrity that’s lost will depend on the type of ceramic and fabrication method used. But, unfortunately, the wide variety of techniques in use today makes this a difficult subject to create general rules and guidelines about.
Our thoughts about the need to replace all-ceramic crowns that have had access cavities made through them.
High-strength dental ceramics.
It would be our interpretation of the articles that we’ve seen that “milled” (monolithic) crowns using newer higher-strength ceramics (like zirconia or lithium disilicate “Engineered” dental “porcelains.”) may retain the greatest level of strength after their root canal access cavity has been patched. Especially those that have been cemented to their tooth using an adhesive technique (a “dental bonding” type of cement). (Bompolaki, Mallya)
But the use of high-strength ceramics in monolithic form is a relatively new phenomenon in dentistry. And as such, it would be our guess that these specific types of restorations represent a relatively small percentage of the total number of all-ceramic crowns found in patients’ mouths.
Of course, the way to know definitively what type of restoration has been placed is to ask the dentist who provided it. Their records will also make mention of the type of luting agent (“cement”) that was used. Other than this source, the full details about your crown probably can’t be known.
Is thorough evaluation even possible?
It caught our eye that the paper by Wood mentions that: “The visualization of crack formation on access (meaning at the time when the access cavity is made) should assist the clinician in the decision to remake the crown.”
▲ Section references – Bompolaki, Wood, Mallya
b) The extent of the access cavity will be a factor too.
It can be that when making the procedure’s access cavity the tooth becomes so hollowed out that it no longer provides a solid foundation for its existing crown. For example, when root canals inside a tooth are difficult to find the dentist may end up trimming away more internal tooth structure than is usual.
A study by Heydecke determined that simply filling in this type of extensive hollow space with dental restorative did not restore tooth strength. So with these types of cases, a new crown (with a more encompassing design and possibly a post and core What’s this?) will need to be made.
▲ Section references – Heydecke
2) Can the existing crown be inspected adequately?
Despite both clinical and x-ray evaluation, a dentist’s interpretation of the status of an existing crown may not be accurate.
- A study by Abbot examined 245 teeth both before and after their dental crown was removed.
- Its findings were that 56% of the time tooth decay, cracks or other defects were not detected during the tooth’s initial evaluation.
3) Can reusing the original crown create an adequate seal for the tooth?
The benefit of just placing a filling.
This solution is a very cost-effective one, in the sense that a repair is made simply and quickly for just the price of a filling as opposed to a new dental crown. However, there are concerns with relying on this type of patch.

Sealing a crown’s access cavity with a filling has both advantages and disadvantages.
Concerns about the success of the tooth’s root canal treatment when a crown is patched.
A big concern associated with root canal treatment that has been performed through a dental crown is whether the patch that’s placed afterward (the filling) can provide an adequate seal. That’s because the crown’s seal over the tooth plays an integral role in helping to ensure the success of the tooth’s endodontic work.
Coronal leakage – A cause of root canal failure.
Following root canal therapy, one very important function that having a crown on the treated tooth provides is that it creates a seal over the tooth that helps to prevent coronal leakage A cause of root canal failure.
This phenomenon is a process where bacteria and debris are able to seep back into the tooth’s interior and recontaminate and reinfect its once-cleansed and sealed root canal space.
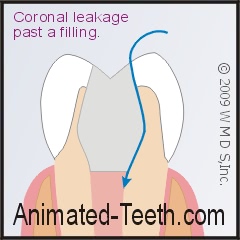
If the integrity of the filling’s seal is lost, bacteria can recontaminate the tooth’s root canal system.
This scenario (and the tooth infection that results) is increasingly recognized, especially by endodontists, to be a significant cause of root canal therapy failure. And if you’ve had your tooth’s work performed through your tooth’s existing crown, you owe it to yourself to read our page linked above. The long-term success of many teeth has been compromised by overlooking this risk.
What’s needed to help to ensure a successful outcome?
When a tooth’s root canal treatment has been performed through its crown, for the case to have a successful outlook, the filling that’s placed to fill in the access cavity that’s been made must not only be able to create a substantial barrier to the attempted seepage of oral contaminants into the interior of your tooth but the seal must also be one that is lasting and predictable.
Unfortunately, these characteristics are difficult to foretell, monitor, and/or insure. And if recontamination occurs, your tooth’s root canal treatment will fail and retreatment will be indicated.
So, which makes the best choice after a root canal, new crown placement, or patching the old one?
The alternative to patching an existing crown that’s had root canal treatment performed through it is to just go ahead and make a new one. And this solution probably offers the greatest level of predictability and longevity, and therefore the greatest outlook for success for your case.
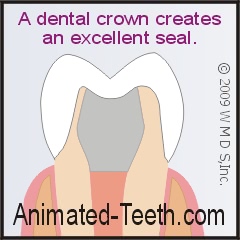
Dental crowns are known for creating effective, lasting seals for completed root canal treatment.
It seems safe enough to suggest that if the amount of time, effort, and money involved with placing a new crown were of no concern (which admittedly they never are), it seems likely that almost every dentist would consider placing a new crown the superior choice.
However, it must also be said that only your dentist knows the facts associated with your case. And in some situations, like those where the access opening is very limited in size and lies in a location where its filling will be subjected to a minimum amount of wear and tear (a situation more commonly associated with front teeth), they may feel that placing a filling will suffice without compromising the outlook for your tooth. You’ll simply have to rely on their guidance.
It may be possible for your dentist to remove your tooth’s crown before performing its endodontic procedure.
Removing a tooth’s dental crown before its root canal therapy is performed, and then recementing it afterward, can be an excellent plan. However, as ideal as this process sounds the practical application of this approach can be quite taxing, both for the dentist and patient alike.
Advantages of crown removal.
a) The integrity of the crown is preserved.
In the case where the crown can be removed fully intact and undamaged, there’s a good chance that it can be permanently recemented after your root canal treatment has been completed. If so, that makes for a very easy and cost-effective solution.
b) Removing the crown aids your dentist’s work.
The new shape that a dental crown can give a tooth can mask its original anatomy and orientation, to the point where interpreting the location of the root canals within can be difficult. If so, the dentist’s efforts to identify and access the canals may result in the removal of excessive amounts of tooth structure or even result in tooth damage.
When the tooth’s crown is removed, it lessens the likelihood of these complications.
Taking off a crown prior to root canal treatment is often easier said than done.
Removing a crown from its underlying tooth in a fashion where it remains fully intact and undamaged can be exceedingly difficult, if not impossible. Despite a dentist’s best and most careful efforts, it’s certainly possible that the crown will be ruined.
Different types of crown construction may favor removal. For example, the brittleness of some types of all-ceramic crowns may make the success of this option unlikely whereas with an all-metal one it might be a possibility. However, even the metal aspect of crowns can be damaged beyond repair during this process.
As an added peril, even the tooth itself might be damaged during the removal attempt, possibly even irreparably.
All of this means that while your dentist can be expected to make a try at removing your tooth’s restoration, if it doesn’t come off easily with their initial efforts they will likely back off fairly quickly for fear of causing further damage. If so, they will then go ahead and drill an access cavity right through the crown. Then, after the tooth’s root canal treatment has been completed, they will evaluate it and its outlook as discussed on this page.
Related pages about restoring root canalled teeth.
- Final restorations – Crown or filling placement after a root canal? The factors that decide.
- Dental post and cores – When is one needed?
- The post and core placement procedure. The steps.
- This topic’s full menu. Go
Page references sources:
Abbott PV. Assessing restored teeth with pulp and periapical diseases for the presence of cracks, caries and marginal breakdown.
Bompolaki D, et al. Fracture resistance of lithium disilicate restorations after endodontic access preparation: An in vitro study.
Heydecke G, et al. Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: an in-vitro study.
Mallya J, et al. Endodontic Access Effect on Full Contour Zirconia and Lithium Disilicate Failure Resistance.
Wood KC, et al. Resistance to fracture of two all-ceramic crown materials following endodontic access.
All reference sources for topic Root Canals.
Video transcription.
Hello. Welcome to Animated Teeth.com and our page that discusses the possibility of reusing a tooth’s dental crown following root canal treatment.
For clarity’s sake, here’s the scenario this video addresses. You have a tooth that has a dental crown on it. Your dentist reports to you that the tooth now requires root canal treatment. So, after its endodontic therapy has been completed will the original crown still be satisfactory or will a new one need to be placed?
As you’ll discover during this video, it all depends on whether or not the original crown can be counted on to provide a reliable seal for your tooth’s root canal work. In explaining further, let’s first investigate a situation where one might.
Consider this scenario. Before performing your tooth’s root canal therapy your dentist removes its dental crown. They then perform your procedure. When finished, they cement your crown back on.
In this case, since the crown hasn’t been altered, and has been cemented back into place, it once again creates a protective seal over your tooth. Its requirements for your tooth are met.
Now, consider this second scenario. Your tooth requires root canal treatment. Instead of removing your tooth’s crown to perform this work, your dentist gains access to the interior of your tooth by way of drilling a hole through it. Your root canal procedure is then performed and completed. The question now becomes, can your existing crown, which now has a hole in it, still be counted on to provide an adequate seal for your tooth?
Well, with this crown there would be a question if it can. And as an answer, yes, possibly it can be reused and provide satisfactory service but making your tooth a new crown really makes the safer, more predictable bet.
Let’s backtrack just a little. As a first question to what we’ve stated so far in this video, you may wonder why all crowns aren’t just removed from their teeth before their root canal treatment is performed.
Well, removing a crown from a tooth can be difficult, possibly exceedingly so. And it’s not uncommon that during the attempt the crown may be irreparably damaged, possibly the tooth too.
So, a dentist may try to remove a crown but if it doesn’t come off easily, they’ll probably back off from this plan pretty quickly.
As a second question, how about the situation where a hole was drilled through the crown? When can that crown still be used?
With this scenario, the primary issue is whether or not the hole can be sealed up, like by placing a dental filling.
As background, the importance of the seal is this. If contaminates, like bacteria and debris, can seep back into the interior of your tooth, its root canal treatment will fail. This phenomenon is referred to as “coronal leakage” and on our website we have a page and video dedicated to just this issue.
So, take the case where a filling has been placed to plug the hole in your crown. Will it create a substantial enough seal? And how long will the seal last, after all, fillings do deteriorate over time.
Well, no one can answer these questions for certain. Your dentist can advise you, based on their impression of your case and their experience with others. And sometimes just plugging the hole with a filling may make a reasonable choice.
However, if the time and cost of making a new restoration for your tooth are of no concern, which of course is seldom the case, the predictable seal that a fully intact crown can offer certainly makes a very attractive, almost always preferable, option. So, talk to your dentist. Let them explain the pros and cons as they apply to your case so you two together can make a decision.
As a second issue, the kind of crown that was previously made for your tooth may be an important influencing factor.
Consider this. Drilling a hole through an all-metal crown, like a gold one, probably won’t weaken it significantly.
The same can probably be said for porcelain-fused-to-metal crowns. Even though the act of drilling the hole may, unpredictably, lead to porcelain fracture sometime in the future, which often will cause a need for crown replacement, the metal layer that encapsulates your tooth will remain intact and continue to provide a seal for its root canal work.
The greatest concern would be with all-ceramic crowns. Some kinds of all-ceramics are astoundingly strong. Others, not nearly so.
With any all-ceramic but especially the latter kind, the act of drilling a hole through the crown might crack it, probably without your dentist realizing it.
A generally intact but cracked ceramic crown might allow coronal leakage to occur. And certainly if the restoration outright fractures, the tooth’s protective seal will be lost.
Once again, only your dentist can advise you, based on their impression and experience, about how much risk you run. Let them explain the pros and cons of your situation so you together can come to a decision about whether your existing crown should continue to be used or not.
We will point out that by now you can probably see that making a new crown offers a lot of advantages, especially in regard to predictability, with the main disadvantage primarily being cost. Of course, after just having had to pay for root canal treatment, we certainly understand how yet another major expense can pose a substantial burden, and how that might make the hope of reusing your existing crown very attractive.
So with those points left for you to quiz your dentist about, we’ll end this video. We’d be remiss in not pointing out that our page contains additional pertinent information about this subject, so be sure to give it a read. Good luck, and goodbye.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Reason not to reuse crown.
The opening in my existing porcelain metal crown seems small to me. Why can’t my dentist just put a white filling in to fill it in and be done with it?
jb
Reply –
We’re not necessarily saying that that can’t be an option. But we can say that making a new crown has some advantages.
1) You state that your existing crown is a porcelain metal one (we’re assuming you mean porcelain-fused-to-metal or PFM).
To access the interior of your tooth your dentist has had to drill a hole through its porcelain layer. That makes the porcelain inherently unstable and more prone to fracture. Probably in most cases this never becomes an issue but the potential is there.
While only cosmetic in nature, we’ll also state that it’s unlikely that the color of the filling placed will exactly match your crown. White filling material (dental composite) has some degree of translucency, which means that it will display some of the color of adjacent materials. In this case, it will have a grey tint due to the adjacent metal layer underneath the crown’s porcelain surface.
2) The most important reason why a new fully intact crown makes the better choice is because of the seal it is able to create over the tooth (see our discussion above about coronal leakage).
When a filling is used to plug the hole, the quality of the seal it creates for the tooth is difficult to evaluate and monitor.
Probably the best thing that the dentist can do in this case is extend the filling down inside the tooth as far as they can (even down into the openings of the actual root canals). This way the filling’s seal is as long as possible, thus creating the most substantial barrier possible.
If the seal is compromised, since your crown has a metal component that covers over the tooth there is no way for the dentist to monitor what’s going on inside (like to check for decay) via x-rays.
All and all, predictability of its seal over the tooth is the main advantage that a new crown offers over just plugging the hole in the existing one with a filling.
Staff Dentist
Comment –
Filling material.
Tooth #29 has a ceramic crown, with a bridge to #27, so I don’t think replacing the crown is an option for me after the root canal. What is the most durable “white tooth bonding” filler material I could use for the access cavity? Thank you!
sb
Reply –
Clearly this is an issue for your dentist to decide but in general terms:
Dental composite products (white filling materials) are manufactured using different formulations. Some of these are made specifically for applications, like restorations for back teeth, where compressive strength and wear resistance are needed.
So at least at the surface of your crown’s opening, they will probably choose a “posterior” dental composite.
What they do inside the tooth is important too. If the filling isn’t just all one piece, they’ll need to make sure that any base materials underneath the restoration (filling in between the filling and actual tooth structure) have good compressive strength characteristics too, so it is adequately supported.
Staff Dentist
Comment –
Root Canal with a Crown
After a root canal has been performed that has a crown on the tooth, can I expect some pain and discomfort until the new crown is replaced.
GS
Reply –
No. Generally that is not correct.
If for some reason the “bite” of the original crown is different than before, then yes that could irritate your tooth. But short of that, the issue of a crown, new or old, would probably have little to do with any near-term postoperative sensitivity you notice.
This page discusses common causes of post-root canal treatment sensitivity.
Staff Dentist
Comment –
Drilling through different types of crowns
Hello. Thank you for this fantastic website. I have found the information to be very helpful. I’m afraid that I might need to have a root canal performed on a crown that was only placed a month ago. The dentist said at first that he was going to order me a crown made of zirconia, but then later referred to it as porcelain when he was putting it in. Does this suggest that it is some sort of hybrid? How will this crown hold up if I get a root canal performed by an endodontist (using smaller, more precise equipment)? Thank you for your time.
Chad
Reply –
You’ll probably have to ask to know for sure.
The best case for your situation is where your crown is a monolithic zirconia crown (a crown milled out of a single block of Zirconia ceramic).
Another type of “Zirconia” crown is one where only the portion of the crown that covers over the tooth is made out of Zirconia. Then on top of this another kind of “porcelain” is layered or pressed on so to give the crown its tooth-like shape. (This is referred to as a veneered Zirconia crown.)
As this paper describes:
Effect of endodontic access cavity preparation on monolithic and ceramic veneered zirconia restorations.
As compared to the veneered form, the monolithic construction form tends to be less damaged by the act of creating the access cavity through the crown.
An endodontist won’t necessarily try to perform your root canal through a smaller access cavity, because having adequate access is key to the success of the procedure. But yes, their skills/equipment/dexterity may be such that they routinely tend to work through a smaller opening.
Also, an endodontist is more likely to know how large of an opening they actually do need. Or in the case of searching for difficult to find canals, be more effective in locating them without removing excessive tooth/crown structure.
Staff Dentist
Comment –
CAD/CAM crown
Hi. Thank you for this website. It is very helpful. I had a cad/cam crown placed on a molar 3 months ago. It was a tooth that had a big old metal filling that was preemptively removed, leaving the remaining tooth quite exposed. After much consideration and waiting, my dentist finally decided to do the cad/cam crown.
Now this is my situation: I think I will probably need a root canal because of the type of pain I started to feel recently. Can a cad/cam crown have an access cavity made through it? Is the structure good enough? Will I be able to keep the crown?
Sofia
Reply –
Per our revision of the information stated above:
The more-ideal construction type is a monolithic (CAD/CAM) crown made from either zirconia or lithium disilicate (the generic names for those materials). Preferably the crown has been cemented using an adhesive process. Your dentist will be quite familiar with all of those terms and can put your mind at ease.
Staff Dentist
