Looking for information about other Dental Topics?
Full Website Index• Animated-Teeth.com •
Problems (pain, sensitivity) associated with permanent and temporary dental crowns. | Treatments and remedies.
Guide to common problems with crowned teeth.
If you have a tooth that has been crowned and have started to notice issues with it, you’re not alone. Whether your crown was placed recently or has been problem-free for years, complications can arise over time.
This guide explores common problems that may develop with crowned teeth, from minor bite misalignments to temperature sensitivity to more serious concerns like abscesses that cause pain and swelling. You’ll also learn about key warning signs to look out for, common causes for what you’re experiencing, and the most effective remedy or treatment for each issue.
We also discuss the unique, usually minor, problems that can occur with temporary crowns and how to address them effectively.
Guide to crowned tooth problems, by symptom.
If you’re reading this page, you’ve probably already noticed problems with your tooth. This section of our guide can help to steer you to the information you need, based on the symptoms you have noticed.
a) Common problems associated with teeth that have permanent crowns.- Tooth pain – Ache, throbbing, pain when biting.
- Sensitivity – Thermal (hot/cold), sensitivity to air.
- “Bite” issues – Irregular bite, tenderness when biting.
- What to do if a permanent crown comes off or you swallow it.
b) Common problems associated with teeth that have temporary crowns.- Gum tissue pain or sensitivity.
- Abnormal bite.
- Sensitivity to hot, cold or air.
- Tooth pain or sensitivity following the crowning procedure.
- What to do if your temporary crown comes off.
- Temporary crown dos, don’ts and precautions.
If you notice problems, you need to let your dentist know.
While we hope you find the contents of this page helpful in understanding what’s possibly taking place with your tooth, bottom line, if you’re having problems of any sort, the right solution is always to contact your dentist so they can evaluate your situation and provide the assistance you require in a timely fashion.
There is no substitute.
Dentists train for years in school and spend small fortunes on equipment all so they can diagnose and address the issues we discuss on this page.
Just reading content on a website is no substitute, nor in most cases will you be able to provide adequate treatment on your own. The types of problems and complications discussed on this page typically require attention from your dentist.
Suboptimal treatment access.
Due to extenuating circumstances, like the 2020 Coronavirus pandemic, some people may find the possibility of appointing with their dentist severely limited or even impossible.
Establishing telephone contact is important.
Even during these uncertain times, all dentists should still have some mechanism in place for assisting with their patients’ dental emergencies.
Initially, this may only be telephone contact. But fortunately, some of the crown-related problems discussed on this page can be diagnosed with some certainty via a phone conversation. And dealt with, at least on a short-term basis, with a home remedy or even just reassurance.
Of course, others cannot. But even some of the most serious conditions discussed below (like infections) can be managed by a dentist via telephone consultation and phoning in a prescription for their patient. So don’t hesitate, establish communication with your dentist early on in case it’s needed in lieu of the possibility of direct treatment.
A) Common problems, pains, sensitivities associated with teeth that have permanent dental crowns.
(The assumption with our discussion here is that the crowned tooth has no obvious extraneous issues, such as tooth decay, or the tooth itself has no issues with gum disease. Instead, the status of the crowned tooth is one where it would seem to be good order but instead painful symptoms exist.)
1) Endodontic complications (nerve problems) with crowned teeth.
The nerve inside a tooth (its “pulp”) is living tissue. And in cases where it’s been repeatedly or severely traumatized, either currently or historically, it may begin to degenerate (die).
Dentists refer to this situation/process as irreversible pulpitis (meaning a state of inflammation from which the tooth’s nerve tissue won’t healthily rebound). And as this condition progresses, symptoms frequently develop, including pain.
Signs and symptoms.
The types of discomfort associated with a tooth that has irreversible pulpitis can be quite varied.
- The level of pain can range from just slight tenderness, or intermittent discomfort that only lasts for a few minutes at a time, all of the way up to a severe toothache that lasts for hours on end.
- The discomfort may be triggered by a stimulus, such as the pressure of biting down, hot foods and beverages, or possibly even cold ones. Once set off, the pain characteristically lingers (as opposed to quickly fading after the stimulus has been removed).
In other cases, the pain may occur spontaneously (on its own, unprovoked).
- The nature of the pain can be quite varied. It can be sharp or dull, localized or diffuse. The pain may have a throbbing, sometimes radiating, nature.
Due to these variations, the patient’s dentist will need to look for additional indications Signs / Symptoms associated with the tooth before being able to conclusively arrive at this diagnosis.
As far as the timing of this complication, pretty much anything is possible.
- Symptoms may first be noticed during the time frame of the crowning procedure (such as following the tooth’s preparation appointment, while its temporary crown is worn, or shortly following the placement of its permanent crown).
- With other cases, the degenerative nature of the pulpitis may take days, weeks, months or possibly even years before it’s progressed to a point where it causes noticeable symptoms.
▲ Section references – Torabinejad
Treatment.
In the case where it’s determined that the tooth’s nerve has received a level of insult from which it can’t recover (irreversible pulpitis), the required solution will be performing root canal treatment. What does this accomplish?
Why would nerve problems just crop up with a crowned tooth?
Crowns aren’t usually placed on pristine teeth. – Instead, they’re usually used to rebuild or strengthen those that have already experience some type of catastrophic event, such as fracture, tooth decay or a lost filling.
These same events can have a detrimental/traumatizing effect on the tooth’s pulp tissue (be a cause of irreversible pulpitis). It may, however, take time for the symptoms associated with the nerve’s problems to show up. And for that reason, a tooth that previously seemed just fine, either before its crowning process was begun or even many years after its crown was placed, may suddenly begin to hurt.
▲ Section references – Rosenstiel
For more information on this subject, this link discusses teeth that have been crowned and later on require root canal treatment. What’s the relationship? And this page, provides ideas about how this type of scenario might be avoided altogether: 8 things you can do to reduce your chances of ever needing a dental crown. Proactive steps.
2) Pain associated with crowned teeth that have failed root canal treatment.
Despite a dentist’s best efforts, some root canal cases will fail. Possible reasons why. And in many cases, one of the signals that a tooth’s has is transient pain or a toothache. Additional signs and symptoms.
Treatment.
In most cases, the tooth can be retreated. Options. However, if the dentist doesn’t feel that the procedure’s chances for success are good, they may instead recommend extraction and replacement. Options.
3) Pain associated with crowned teeth that have cracks.
Crowns generally create a splinting effect How they do this. that helps to hold teeth together. But it’s possible for a crack to develop, or an existing crack to continue to grow in size, in the tooth’s root beyond where its stabilizing forces are effective. If so:
- When pressure is applied to the tooth, the two split halves may move independently, thus causing pain.
- The crack may harbor bacteria. Or it may provide a pathway for them to enter the tooth’s root canal system, thus compromising its nerve tissue (cause irreversible pulpitis).
Signs and symptoms – In regard to discomfort, cracked teeth characteristically give a sharp, painful response to pressure changes (like when biting down, or letting biting pressure off a tooth).
▲ Section references – Torabinejad
4) Problems with a crown’s “bite” that can cause pain.
a) “Bite” issues with a new crown.
While your dentist will evaluate the way your new crown bites against the teeth it opposes, you may discover (especially after your numbness has worn off) that its shape still isn’t quite right.
As examples:
- You may find that it touches prematurely (first) when you bring your teeth together. This is referred to as the crown being “too high”.
- Or maybe as you slide your teeth together from side to side, you can feel some aspect of the crown that’s too prominent.
Pain – Symptoms and causes.
- Initially, you may just notice slight tenderness with either the crowned tooth or the teeth that bite against it. If the situation is allowed to persist, severe pain may be experienced.
- The source of the pain is generally two-fold. The continued trauma both inflames the ligament that binds the involved teeth in their sockets, and their nerve tissue (reversible pulpitis). The hypersensitivity that you notice is a symptom of this inflammation.
Treatment.
- If treated early on, this type of problem is an easy fix for your dentist. They simply need to buff your crown down so its shape is more in harmony with your bite. After that’s been accomplished, the tooth’s condition (reversible pulpitis) should settle down.
- Don’t expect this type of problem to just take care of itself because it won’t. In fact, if this condition is not remedied in a timely fashion your tooth can become very sore.
- We discuss the use of medication with this complication below.
▲ Section references – Ingle, Koch
b) Painful “bite” issues associated with existing crowns.
It’s possible for teeth that were crowned some time ago, even those that have always seemed just fine, to develop some type of painful bite-related issue.
1) Individual crowned tooth pain related to tooth grinding.
It may be that the “bite” of a crown is very close to perfect. And as such, all is well with the tooth most of the time.
But during periods when the person bruxes (clenches and grinds their teeth), especially for extended periods of time and with heavy force, the minute prominent aspects of the crown direct excessive forces to its tooth.
If so, the consequences will be inflammation of its nerve tissue (pulpitis) and the ligament that binds the tooth in its socket, and ultimately some level of sensitivity, hypersensitivity or pain.
Treatment.
This condition is very similar to the discussion above about when a crown is too “high.”
- In routine cases, the dentist will buff the chewing surface of the crown down so it’s in harmony with the person’s bite. The tooth’s sensitivity should then settle down, often quite promptly.
- (More details about how this condition is managed.)
2) Tooth infections.
Infections of endodontic (inside the tooth) or periodontal (involving the supporting tissues of a tooth) origin may cause a tooth that has a dental crown to be sensitive to biting pressure. However, the level and characteristics of what’s noticed can be quite varied and lie beyond the scope of this page.
It should be stated that it’s possible for these types of infections to be the cause of a person’s discomfort, without the tooth and it’s neighboring tissues necessarily displaying other obvious signs (like swelling).
Treatment – After diagnosis by your dentist, the solution is to resolve the conditions that have allowed the formation of the infection, either by way of performing root canal therapy or a periodontal (gum) procedure.
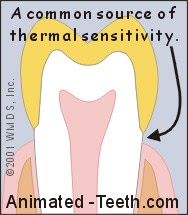
Crown thermal sensitivity may come from sensitive tooth surfaces at its edge.
5) Crowned teeth that experience sensitivity to hot, cold or air.
a) Routine cases.
- Hot and cold foods and beverages. (“Thermal” sensitivity.)
- Air. (Like when breathing in and out through your mouth.)
- The location of the sensitivity is usually right at the edge of the crown, by the gum line.
- The pain is triggered by the hot, cold or air stimulus but then disappears. It’s typically just mild to moderate in intensity. What’s felt is always about the same. It doesn’t worsen.
It’s possible for this condition to crop up with older (existing) crowns too.
Exposed tooth dentin can explain thermal pain.
Yellow = The dentin portions of a tooth.
Routine causes of this type of sensitivity.
The exposed dentin may exist because the enamel layer that originally lay over it was trimmed away when the tooth was shaped for its crown. Or else the exposed surface of the tooth is its root (a portion of the tooth that has no enamel covering).
- In the case of a new dental crown, the sensitivity may be a sign that the restoration doesn’t cover over the tooth quite as fully as it ideally might.
(The band of exposed dentin surrounding the edge of the crown may be so minute that the discrepancy can’t even be visualized. Note: Having this problem doesn’t necessarily mean that the crown is poorly made or deficient.)
- With existing crowns, developing sensitivity is frequently due to gum recession.
(As the tooth’s gum tissue recedes, potentially sensitive root surfaces become exposed. Even very minor amounts of recession can result in sensitivity.)
Treatment.
- The cure might be as simple as using toothpaste that’s marketed as a treatment for “sensitive teeth” (the active ingredient in these products is usually potassium nitrate).
- Or the dentist may treat the exposed dentin with a “desensitizing” application. Examples include tooth varnish or else fluoride.
▲ Section references – Rosenstiel, Yadav
b) More problematic conditions.
Beyond routine exposed-dentin sensitivity (the condition just discussed), there can be other explanations for a crowned tooth’s sensitivity to air or hot/cold stimuli.
- A crowned tooth whose nerve tissue is inflamed (reversible or irreversible pulpitis) may respond painfully to these stimuli.
- Crowned teeth that are in need of root canal treatment might display these symptoms too.
- Post cementation sensitivity may also lie at fault. (The type of cement, or protocol used, to permanently cement a dental crown may result in sensitivity.)
▲ Section references – Chandrasekhar
B) Common problems, pains, sensitivities associated with temporary dental crowns.
Teeth that currently have a temporary (interim) crown placed on them A part of the crowning procedure. can experience most all of the same types of pain-related problems as those discussed above with permanent ones.
So instead of rehashing those situations and conditions, this section focuses more so on causes of discomfort that tend to be side effects of the crowning procedure, or pains or sensitivities related to the short-term, disposable nature the temporary crown itself.
Stay in touch with your dentist.
Of course, in all cases when experiencing any type of problem you should report it to your dentist so they can evaluate your situation. This is their obligation to you as your treatment provider.
1) Gum tissue pain.
The edge of most crowns ends right at or below the gum line. And it’s easy for the tissue in this area to get roughed up during the crown-making process (either when your tooth is trimmed, or during the impression taking process).
That means any tenderness you feel along the edge of your temporary crown is less likely related to it, as opposed to the adjacent irritated gum tissue.
Treatment.
In most cases, you can expect that this type of discomfort will resolve on its own after a few days. Rinsing with warm salt water, up to three times a day, can help to speed up healing.
2) Pain and tenderness associated with a temporary crown’s “bite.”
After the numbness of your procedure has worn off, you may notice that something is amiss with the “bite” of your temporary crown. For example:
- When you close your teeth together, it may seem too tall (as in it touches first as you bring your teeth together, possibly keeping you from closing all of the way).
(In dentist terminology, the temporary crown is referred to as being “too high.”)
- The “bite” may seem OK when you initially close. But as you slide your teeth left, right or forward, the shape of the temporary deflects your normal jaw movements.
- Initially, the tooth may not hurt very much at all. But as time goes by, it may become more and more sensitive, or be outright painful.
The cause of the problem.
The fundamental problem is simply that the shape of the temporary crown isn’t quite right. And having this complication is not all that uncommon.
The dentist’s inability to get the “bite” right usually stems from either:
- Patient confusion in following instructions about what type of jaw movements to make during testing.
- The patient’s inability to create the needed movements due to the feeling of numbness they are experiencing.
The pain itself is due to inflammation of the tooth’s nerve (reversible pulpitis) and/or the ligament that binds it in its socket, caused by the constant trauma caused by the heavy bite.
Treatment.
If tended to early enough, this is a simple problem to fix. Your dentist just needs to buff down the surface of your temporary with their drill, so it’s more in harmony with your bite. (Doing so should just take a few moments.)
- If you’ve had discomfort, your tooth will usually return to normal promptly. In some cases, it may take a day or two. (The condition involved being reversible pulpitis.)
- It’s common for a dentist to recommend the use of an over-the-counter NSAID medication (non-steroidal anti-inflammatory drug) such as Ibuprofen, Motrin or aspirin. (Details on the use of ibuprofen.)
This class of pain relievers provides the added benefit that they also help to limit the extent of nerve tissue inflammation that takes occurs, which assists the tooth in making a healthy recovery from the episode.
3) Teeth that have increased thermal sensitivity.
Teeth fitted with a temporary crown sometimes exhibit sensitivity to:
- Air. (Like when you breathe through your mouth.)
- Hot and cold foods and beverages. (Dentists refer to this as thermal sensitivity.)
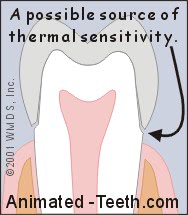
A temporary crown may have a fairly imprecise fit, thus explaining its thermal sensitivity.
a) A possible simple cause of the sensitivity.
If so, hot or cold stimuli or air may irritate it, resulting in the sensitivity that you feel.
Treatment.
After an evaluation of your situation, your dentist will determine what level of attention is required. They may decide that your temporary crown needs additional work, or even replacement. Or that the application of a liquid coating (tooth varnish) over the exposed dentin will control the problem. If what’s noticed is just minor, it may not be treated.
b) More problematic conditions.
A crowned tooth whose nerve tissue is inflamed (reversible or irreversible pulpitis) may respond painfully to hot and/or cold stimuli, possibly even air. Crowned teeth in need of root canal treatment might too. We’ve discussed these conditions above on this page.
4) Tooth pain following the crowning procedure.
It’s possible that following your appointment when your tooth was trimmed/shaped for its dental crown Crown procedure steps., it will start to cause discomfort.
With this scenario, it may be that your tooth currently has a temporary crown on it. Or in the case of single-visit protocol “1 hour” crowns., your tooth’s permanent crown may have already been cemented.
Possible causes of this type of sensitivity.
In most cases, the discomfort is due to inflammation of the tooth’s nerve tissue (a “pulpitis”) that’s been triggered by trauma created during the crowning procedure.
The issue of concern being, how extensive the tooth’s reaction will be, and how it will ultimately affect its health and outlook.
a) Reversible pulpitis – This is the case where the resulting inflammation is just transient and reversible, meaning it will ultimately resolve and the tooth’s nerve tissue will return to a normal, healthy state. And in most cases after a tooth has been trimmed for a crown, this is the outcome that can be expected.
Potentially useful medications.
To assist the tooth’s nerve in settling down and recovering, and to help to minimize the amount of pain you feel as it does, your dentist may recommend that you take an over-the-counter NSAID medication (non-steroidal anti-inflammatory drug) such as ibuprofen (Motrin, Advil), aspirin, naproxen (Aleve). (The appropriateness of the use of any drug by a patient must of course be evaluated first.)
The medication is typically taken over the few days it takes for the tooth to gradually return to normal. Doing so can be an important step in helping your tooth to recover, and therefore prevent the added complications (time, expense, toothache) that dealing with irreversible pulpitis typically presents.
- As an example of an adult’s use of ibuprofen with the goal of reducing pulpal inflammation so to aid the tooth in making a healthy recovery, with the added benefit of controlling discomfort: 200 to 400 mg every 6 hours for 1 to 3 days as the tooth’s symptoms subside.
▲ Section references – Haas, Hargreaves
b) Irreversible pulpitis – This is the situation where the trauma associated with trimming the tooth for its crown has pushed the tooth’s nerve “over the edge.”
The resulting inflammation has created a situation from which the nerve tissue can’t recover. With this scenario, the ultimate outcome will be one where the tooth will require root canal therapy.
Treatment.
Since the range of outcomes between these two conditions is so great, if you notice pain or discomfort you need to be in touch with your dentist, and sooner rather than later.
- Following simple steps that they recommend, such as taking an anti-inflammatory drug (NSAID) early on, may help to prevent the condition of irreversible pulpitis from developing.
- Once having been alerted, your dentist can monitor your condition, help to manage your symptoms and provide prompt attention if your status worsens.
(This link discusses the the crowning procedure and the possible need for root canal treatment as a result What’s the relationship? in greater detail.)
If your tooth is sensitive, your permanent crown’s placement should be delayed.
It’s important that your tooth is asymptomatic (or at least its symptoms slight and easily explained) at the appointment when your temporary crown is taken off and your new permanent crown is cemented.
The nature of some types of crowns (especially those that have a metal component that conducts hot and cold), and the cementation process associated with placing your permanent crown (which may aggravate a tooth, see above), may place you at risk of experiencing continued, or even increased, sensitivity.
▲ Section references – Shillingburg
What should you do if your permanent or temporary dental crown comes off?
We now discuss these topics on the following pages:
- What to do if you’ve had a dental crown fall out. Jump to page.
- What to do if you’ve swallowed your crown. Jump to page.
Precautions to take with temporary dental crowns.
What kind of service can you expect from your temporary?
Generally speaking, properly executed provisional crowns rarely fail. Loss or fracture is usually associated with deficiencies involving either the tooth’s preparation (shape) or the temporary’s construction.
▲ Section references – Schwass
Remember, your temporary crown has been cemented using temporary cement.
A temporary dental crown is usually cemented using “temporary” cement, so it can be removed easily at that appointment when your permanent one is placed.
And since this kind of cement is not as strong as others, your dentist will probably recommend that you take the following precautions. (Ask them if there are any other steps that they feel are important for you to take too.)
1) Favor the side of your mouth that has the temporary.
There’s no need to look for trouble, so give your temporary crown some consideration when eating. As much as possible, shift the bulk of your chewing activities to other areas.
2) Keep sticky foods away.
Anything sticky (caramel, chewing gum, etc…) has the potential to grab onto your temporary crown and pull it off.
3) Avoid hard foods.
Exceptionally hard foods, such as raw vegetables (carrots), can break or dislodge a temporary crown.
4) Be careful when you floss.
A tooth that has a temporary can usually be flossed in normal fashion How to., with the following consideration.
When finished, it may be best to remove the floss by way of letting loose of one end of it and then pulling it out to the side. Pulling the floss back up and out in normal fashion might snag the edge of the crown and pull it off.
Page references sources:
Chandrasekhar V. Post cementation sensitivity evaluation of glass Ionomer, zinc phosphate and resin modified glass Ionomer luting cements under class II inlays: An in vivo comparative study.
Haas BA. An Update on Analgesics for the Management of Acute Postoperative Dental Pain.
Hargreaves K, et al. Drugs for pain management in dentistry.
Ingle JI, et al. Ingle’s Endodontics. Chapter: Pulpal Pathosis.
Koch K, et al. How to avoid your worst endodontic disaster.
Rosenstiel SF, et al. Contemporary Fix Prosthodontics. Chapter: Principles of tooth preparation.
Schwass DR, et al. How long will it last? The expected longevity of prosthodontic and restorative treatment.
Shillingburg HT, et al. Fundamentals of Fixed Prosthodontics. Chapter: Tryin and adjustment of gold restorations.
Torabinejad M, et al. Endodontics. Principles and Practice. Chapter: Pulp and periapical pathosis.
Yadav K, et al. Dentin hypersensitivity following tooth preparation: A clinical study in the spectrum of gender.
All reference sources for topic Dental Crowns.
