Types of tooth discoloration – Organized by color, appearance, and underlying cause.
The color and appearance of tooth staining can usually give you a pretty good idea of what has caused it.
This page explains what to look for when making a determination (stain location, extent, surface texture, hue/tint, etc…). And then, details teeth whitening methods that can be used as a solution for that kind of discoloration.
Types of tooth discoloration and their causes –
Agent/Cause, General appearance –
- Chromogenic compounds (foods, beverages, other consumables) –
The dark compounds found in products we consume (coffee, tea, cola, wine, tobacco, etc…) can cause yellow, brown, or burnt orange tooth staining.
In most cases the discoloration is generalized, meaning that it tends to affect all teeth and tooth areas somewhat equally.
[More details, pictures …]
- Age-related darkening –
It’s normal for a person’s teeth to gradually take on a generalized yellow or brown coloration as years and decades pass.
[More details, pictures …]
- Genetic factors –
The baseline color of a person’s teeth may naturally be more yellow, brown, or gray, or relatively lighter or darker, than other people due to their particular genetic make-up.
[More details, pictures …] - Tetracycline (and related antibiotics) –
Tetracycline tooth stains can be yellow-brown or possibly blue-grey in color.
The pattern of the staining can be quite varied. It can appear as isolated areas or lines but more likely involves broad bands or whole-tooth discoloration. Characteristically, multiple teeth are affected.
[More details, pictures …] - Fluoride (fluorosis) –
Fluorosis staining results in chalky-white or possibly brown spots, patches or lines dispersed across a tooth’s surface. The blemishes may show evidence of surface pitting. Typically, multiple teeth are involved.
[More details, pictures …]
- Internal tooth changes / Root canal treatment –
Generalized brown or gray discoloration can be caused by changes that have occurred within a tooth’s nerve space. The process can be triggered by events such as trauma or needing to or having had root canal treatment. Only those teeth directly affected by the event (frequently just a single tooth) are affected.
[More details, pictures …] - Tooth decay –
The early stages of cavity development result in the formation of white spots or patches on enamel tooth surfaces. The affected area will lose its glossy sheen and on close inspection may show evidence of surface damage.
As the decay process advances, the involved area typically takes on a tan, brown, or black coloration. The lesion itself may first become noticeable as a small dark spot or blemish that grows in size over time (typically months to years), frequently involving obvious tooth destruction.
[More details, pictures …]
- Deteriorated dental restorations –
Deteriorated or failed dental work can result in areas of yellow, brown, gray, or even black tooth discoloration. A dark spot, line, or underlying halo effect may develop at the edges of the failing restoration. Areas of associated tooth decay may be visible.
[More details, pictures …] - Surface staining (Extrinsic stain) / Poor oral hygiene –
The accumulation of debris on the surface of teeth and/or the staining of it can result in white, yellow, orange, tan, brown, black, or possibly even green discolorations. The staining is typically most intense in those areas that are hardest to keep clean, such as near the gum line.
[More details, pictures …]
Still need some help figuring things out?
If you’re still in the dark about what kind of tooth discoloration you have, working through our list of simple questions Jump to list. can usually help you figure out your condition’s likely cause.
Specific details about types of tooth discoloration.
It’s normal for a person’s teeth to darken over time due to the effects of aging or a perpetual exposure to staining agents (coffee, tea, colas, tobacco, etc).
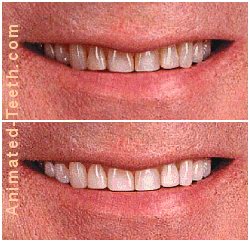
Whitening results at least this good are commonplace.
A) Staining caused by the products you consume.
- The staining effect is caused by dark-colored compounds (like tannins found in tea and coffee, or nicotine in tobacco products) that become trapped within the tooth’s enamel.
- Any consumable that has a strong coloration (such as blueberries, cherries, cranberries, soy sauce) has the potential to cause this effect.
- As a rule of thumb, if you regularly expose your teeth to something that would stain your clothes, it has the potential to darken them too.
It’s a cumulative effect.
The degree of darkening that occurs generally correlates with the regularity and level of exposure that the person has to the agents that have caused it.
Prevention: You may be able to minimize the effects of chromogenic foods by brushing immediately after consuming them. With beverages, try rinsing with water immediately afterward or else drinking through a straw.
Staining pattern.
It’s most common that this type of discoloration will affect all of a person’s teeth somewhat equally. Individual teeth that have white fillings may stain more so.
How to treat / Details
This type of tooth discoloration will usually respond favorably to at-home whitening treatments (tray-based, whitening strips), often surprisingly so. This is especially true for people whose teeth once had a light coloration, as opposed to those whose original baseline shade was always comparatively dark.
Rules of thumb.
- It’s certainly possible that a person will start to see improvement in as little as just a few at-home whitening sessions.
- Teeth that have a yellow to brown tint typically respond more quickly and favorably than those displaying shades of grey.
- For relatively stubborn cases, a realistic treatment time frame can be two to six weeks of daily tray-based bleaching, with each session lasting on the order of two hours.
Darker staining, such as that caused by a person’s heavy smoking habit (nicotine staining), might take upward of three months of treatment to successfully resolve.
B) Systemic exposure to medicinal compounds (tetracycline, fluoride).
If some types of compounds are swallowed by young children (or their pregnant mothers) during that time frame when their teeth are developing, the composition of their mineralized tooth tissues (enamel and/or dentin) may be affected as they form.
If so, the optical properties of these tissues may be altered, thus affecting the color and appearance of the child’s teeth.
Staining pattern.
The exact type or pattern of staining that forms simply depends on: 1) The level of exposure. 2) Exposure duration. 3) What portion of the tooth was forming during that time frame when the child’s exposure took place.
It’s most likely that multiple teeth have been affected. And usually in matching left-right pairs (since teeth on both sides of the mouth will be at the same point in development at the same time).
- Generalized (has affected the appearance of the entire tooth) or else has caused wide bands of staining. – A result of continuous, prolonged exposure to the compound.
- Appear as individual (although frequently multiple) splotches, patches, lines, or ribbons of stain. – A result of repeated, shorter-term exposures.
Severe generalized tetracycline staining.
1) Tetracycline.
This type of staining:
- Is typically yellow to yellow-brown in color, although it can have a blue-grey tint instead.
- The discoloration may affect the entire tooth (as a result of prolonged exposure) or be band-like (if the medicine was administered in courses).
- A diagnosis of tetracycline staining can be confirmed by shining an ultraviolet light (a “black” light) on the teeth, which makes them fluoresce.
Prevention.
As a standard rule, tetracycline (and related antibiotics) should not be prescribed for children eight years and younger, or pregnant women. (Both precautions involve time periods when a child’s teeth are developing.)
Staining with adults.
The long-term use of tetracycline and minocycline has been reported to cause tooth discoloration even in adults. This is a point long after tooth formation has been completed.
This occurs in about 3 to 6% of cases and can affect the root and/or enamel-covered portion of the teeth. For this reason, chronic use of these medicines should be avoided if possible.
▲ Section references – Sánchez
How to treat / Details
Teeth that have tetracycline staining typically have a reputation for being stubborn to treat. There are published case studies that document the use of tray-whitening, and less frequently whitening-strip, techniques to successfully resolve this type of discoloration. But one would have to assume that both the patient and the dentist supervising their efforts were highly motivated to be able to achieve this level of success.
Rules of thumb.
- The greatest chance of success would probably lie with the use of a tray-based at-home system or professional (in-office) treatments, or some combination of both.
- With a tray-based system, the bleaching process should be monitored by a dentist and it may need to involve an extended period of treatment. Durations for difficult cases can easily range between 2 and 6 months, possibly even a year.
- Even with the option of extended treatment, an acceptable outcome may not be possible. For example, after some initial success, a point may be reached beyond which little additional lightening effect takes place.
If so, the dentist and patient may be forced to come to the realization that while the teeth have responded somewhat (or even significantly), achieving any additional improvement is unlikely and the treatments should be terminated.
- If the patient’s bleaching treatments were able to make a substantial yet incomplete improvement in the appearance of their teeth, then those isolated regions on each tooth that didn’t respond (like areas that originally were the darkest) could be masked by placing dental bonding.
If the whitening treatments didn’t even come close to resolving the staining in a manner that the patient found satisfactory, then placing porcelain veneers might be considered.
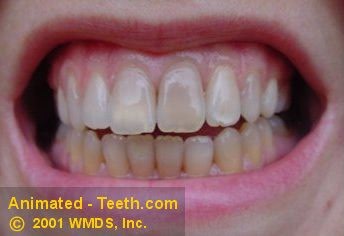
Mild-dental fluorosis. Sometimes called “snow capping.”
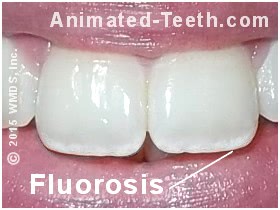
2) Fluoride (fluorosis).
The staining can take the following forms:
- With mild cases, the blemishes are lusterless, chalky-white patches or streaks that run across the surface of the teeth.
Severe fluorosis tooth staining.

- In moderate cases, the color of the staining can be yellow or even brown.
- The pattern of the discoloration frequently shows bilateral symmetry (has affected the same teeth on both sides of the mouth in the same way).
- With the most severe cases, the surface of the affected teeth can be pitted and the teeth themselves malformed.
Prevention. – We discuss fluoride precautions here.
How to treat / Details
- Treating white fluorosis. – Keep reading on. Just below we explain how this condition can sometimes be suitably resolved via whitening treatments.
- Treating brown/dark fluorosis. – These cases are treated similarly to tetracycline staining, discussed above.
- Non-whitening treatment options for severe cases may need to include dental filling (tooth bonding), porcelain veneer, and/or dental crown placement.

Treating fluorosis with whitening treatments.
Treating white dental fluorosis.
Rules of thumb.
- The outcome of this approach hinges on how white the fluorosis is and if the tooth’s enamel can be lightened that much. Success will be easiest for teeth that already have a relatively light baseline color.
- The treatment results can be one where at a distance the color of the teeth looks uniform enough but on close inspection, the individual patches of fluorosis can still be seen.
Even if the final results aren’t perfect, from a standpoint of cost, effort, and the fact that a dental restoration doesn’t have to be placed, they might be considered to be quite satisfactory.
C) Age-related darkening.
It’s normal for a person’s teeth to darken as years and decades pass. Some of this can be attributed to the effects of chromogenic agents such as coffee, cola, and tobacco products (see above). But there’s another reason why it occurs too.
How light enters into and reflects back out of a tooth.
With age, thinner enamel and darker underlying dentin results in tooth darkening.
- Light first penetrates into and through a tooth’s translucent enamel layer.
- Then, when it strikes the tooth’s opaque dentin underneath, it reflects back out.
- With age, the thickness of a tooth’s enamel layer typically becomes thinner, thus revealing more of the comparatively darker dentin that lies underneath.
- The color of a tooth’s dentin tends to change over time. It typically becomes darker as more of it is created within the tooth due to normal physiologic and reparative processes (this is referred to as secondary dentin formation).
Staining pattern.
It would be most common that age-related darkening would affect all teeth somewhat equally.
How to treat / Details
Treatment for age-related staining is the same as for teeth that have darkened as a result of persistent exposure to chromogenic agents (food, beverages, tobacco, etc…), discussed above.
Teeth that have a naturally dark baseline color.

D) Genetic factors. / Inherent baseline color.
Due to their genetic makeup, some people’s teeth may be naturally lighter or darker than others. There can also be color variations that are obvious yet normal. Some people have teeth that tend to be more blue-grey, others more yellow-brown.

Documenting a patient’s tooth shade.
Staining pattern.
It would be most common that color variations due to genetic factors would tend to affect all of a person’s teeth equally.
How to treat / Details
The level of success that’s possible for people who have naturally dark teeth frequently isn’t as dramatic or satisfactory as with other types of tooth discoloration.
Treatments might involve the use of a tray-based system, professional (in-office) treatments, or a combination of both. However, with any of these approaches, the level of improvement that’s ultimately achieved is generally impossible to predict.
Rules of thumb.
- When using a tray-based system, an extended treatment time frame may be required, possibly extending over several months.
- If in-office treatments are used, multiple sessions may be needed.
With either approach, the amount of improvement may fall short of what had initially been hoped.
E) Individual tooth darkening due to internal changes.
Teeth whose nerve tissue has undergone changes, or have had root canal therapy, frequently darken.
This tooth needs root canal treatment.
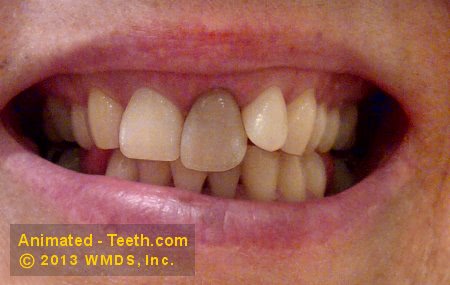
- Yellow-brown to brown-gray.
- In some cases, it may have a pink to purple hue.
- The staining may be uniform, or most intense and darkest nearest the gum line.
As an explanation, some aspects of the staining may be due to:
- In response to experiencing some type of trauma, the tooth may form new layers of dentin within its nerve space. This tends to decrease the overall translucency of the tooth, thus making it appear darker.
Blood cell breakdown compounds leaching into the hard tissues of a tooth cause it to darken.
- Decomposing red blood cells inside the nerve space of a tooth will release iron pigments (due to the breakdown of the iron-rich compound hemoglobin). These dark pigments can penetrate into the tooth’s hard tissues (dentin and enamel), thus causing them to darken.
Red blood cells might be released within a tooth’s nerve space as a result of trauma, or as a consequence of pathology (like nerve tissue degeneration). Likewise, following a tooth’s root canal treatment remnants of blood cells may remain thus causing this type of discoloration to form.
Note: If an individual tooth has darkened, especially one that has a history of receiving trauma (even many years before), it may be an indication that the health of its nerve tissue has been seriously compromised and that performing root canal therapy is now indicated.
Until that treatment has been performed, the potential always exists that the tooth might at some point experience an acute flare-up (pain, swelling). For this reason, any individually darkened tooth should always be evaluated by a dentist.
An individually darkened tooth.

(It needs or has had root canal treatment.)
How to treat / Details
- Professional (in-office) bleaching technique can be modified so the whitener is only applied to an individual tooth.
- Dark teeth that have had root canal treatment are usually lightened using a method where the dentist places the bleaching agents directly inside the tooth.
- At-home paint-on whiteners/whitening pens (a method that can be used to treat individual teeth) are typically ineffective as compared to professional treatment.
F) Tooth decay.
1) White-spot lesions.

White spot lesions resulting from poor home care while wearing braces.
These discolorations are called white-spot lesions, and they’re the earliest visible sign of cavity formation.
- They develop in those areas where dental plaque has been allowed to remain on a tooth’s surface for extended periods of time.
- Common locations are both right at the gum line and around orthodontic brackets.
While they are a stage of cavity formation, they may or may not require attention.
As general guidelines:
- If the enamel surface in the area of the lesion is still hard and smooth, corrective treatment may not be needed.
- If instead the surface is soft or has started to deteriorate, a filling will need to be placed.
Note: Only your dentist has the expertise needed to make this determination.
How to treat / Details
It may be possible to use whitening treatments (whitening strips, tray-based, or in-office treatments) to mask white-spot damage. The attempt is to lighten the tooth’s unaffected enamel, thus making the color mismatch with the white-spot lesion less visible.
What type of outcome can be expected?
- The success of this approach hinges on how light the white spots are and if the tooth’s surrounding enamel will lighten up that much.
- Teeth that already have a light baseline color will typically be the easiest to successfully treat.
- The results can be one where at a distance the color of the teeth looks uniform. But on close inspection, the individual white spots can still be seen.
Even if the final results aren’t perfect, from a standpoint of cost, effort, and the fact that a dental restoration doesn’t have to be placed, they might be considered to be quite satisfactory.
Precautions.
- Before this technique can be initiated, the dentist must first determine that the lesions are inactive and benign.
- It’s important to understand that this approach should never be attempted on your own. Only a dentist has the knowledge and expertise to be able to make the above determination.
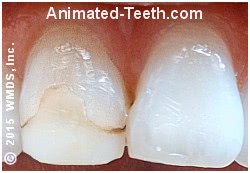
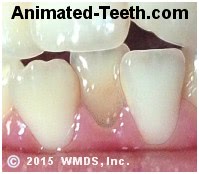
Discoloration due to tooth decay.

The dark areas indicate underlying tooth decay.
2) Cavities.
- The tooth’s surface may show some type of damage or void in the area of the discoloration.
- In other cases, the tooth’s darkened surface hints at the decay that lies underneath. (See picture.)
How to treat / Details
These types of lesions need immediate treatment from your dentist.
G) Dental work.
Some color discrepancies may involve existing dental work.
A deteriorated composite dental filling.
The faint dark line on the left is stain at the edge of the filling. The dark spot on the right is tooth decay.
1) White dental fillings.
Solutions.
As a general rule, teeth whitening treatments won’t change the color of existing dental work (with a few exceptions). So, in the case of white fillings that no longer match, the only solution is to have your dentist replace them.
2) Silver dental fillings.
Over time, metal (amalgam, “silver”) fillings tend to stain the tooth structure that surrounds them. This discoloration usually has a gray-blue tint and can become quite dark.
Solutions.
Teeth whitening treatments cannot be expected to resolve this issue. The only solution is to have some type of replacement dental restoration placed.
The color dental crowns #1 & #3 no longer match.

3) Dental crowns.
That means as a person’s natural teeth undergo a gradual staining process, the dental crown that matched its neighbors perfectly when it was first place will eventually end up looking too light.
This dental crown no longer matches well.

It likely did at the time of its placement, but the color of the natural teeth has since faded.
How to treat / Details
- This approach works because, as a general rule, peroxide-based whiteners don’t have an effect on existing porcelain dental work.
- There are some exceptions to this rule, see our veneers section below.
Precautions.
In some cases, this same phenomenon can also be a detriment. People who initiate whitening treatments on their own (without consulting with their dentist first) may unexpectedly find that their treatments have created a color mismatch between their natural teeth and their existing dental restorations. The only solution is to replace the dental work, which can be both time-consuming and expensive.
4) Porcelain veneers.
The whitener penetrates from the backside of the veneered tooth.
How this works.
- Veneers are translucent shells of porcelain bonded onto the front side of teeth.
- When a tray-based system is used, the whitener can’t penetrate the tooth’s veneered surface but it can its backside.
- Since the tooth does get some dosing of the whitener, there’s potential that it will lighten.
- If the veneer is translucent enough, as its tooth becomes lighter, it will look whiter too.
There can be cases where it is inappropriate to expose porcelain restorations to whitening agents. You’ll need to consult with your dentist on this issue.
H) Surface stains / Extrinsic staining.
Surface staining is discoloration that has built up on the exterior surface of a tooth (hence the term “extrinsic staining”). The underlying tooth itself (its enamel and dentin) still remains the same color it has always been.
This type of discoloration is generally due to the accumulation of dental plaque, calculus (tartar), and/or other assorted debris on the surface of the tooth that itself has a coloration or has become stained. Its formation is characteristically associated with lax or infrequent oral home care and is generally not a problem for those who brush frequently enough (at least twice a day is the usual recommendation), and thoroughly each time.
Surface stain and debris.
The tooth that is hardest to clean has accumulated the most stain.
- Yellow staining may simply be the natural color of heavy plaque and/or tartar build-up.
- Yellow, tan, or brown staining of the accumulation may be due to its exposure to chromogenic agents such as tobacco or dark-colored foods and beverages. (The latter includes cola, red wine, coffee, tea, blueberries, blackberries, etc…)
- Brown staining can also be associated with the use of some medications. As examples, stannous fluoride and chlorhexidine, two medications dentist often instruct their patients to use, are well-known causes of brown surface staining.
- Green and orange tints are most often associated with the presence of chromogenic bacteria living in the plaque accumulation on the affected teeth.
- Black surface staining is less common than other colors and is most notably associated with high iron content in the person’s saliva.
Some common characteristics of extrinsic staining are:
- The discoloration is usually heaviest on that part of the tooth that’s most difficult to clean. (See picture above.)
- The staining can be so adherent and thin that it seems to be a part of your tooth. In other cases, it may have an obvious thickness that’s either hard or soft (or a combination of both).
This black spot is due to a pit in the tooth’s enamel that has collected debris.
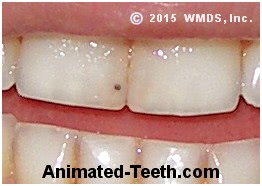
Because this person doesn’t floss, staining has accumulated in between their lower teeth.
Staining pattern.
In some cases, all of a person’s teeth may show evidence of staining. More likely, just certain teeth, or a group of neighboring teeth, are affected.
How to treat / Details
While performing whitening treatments may make an improvement with this type of discoloration, they’re not the needed solution.
This type of stain should be removed via a professional dental cleaning. Afterward, improved oral home care (brushing and flossing) should be able to keep it from reforming (or at least as quickly).
Note: Since surface staining can be confused with or compound the appearance of other types of tooth discoloration, a dentist will usually want to perform a dental cleaning before initiating any type of whitening treatment.
What type of tooth staining do you have?
By answering the simple questions below, you should be able to get an idea of the possible causes of the tooth discoloration you have. You can then use the staining’s associated link to return to our text above for discussion and treatment solutions.
I) The staining has –
a) Always existed.
In most cases, this type of tooth staining is either: 1) Genetic in nature (i.e. naturally dark teeth) or 2) Caused by systemic exposure to compounds that took place while your teeth were initially developing, such as an inappropriate exposure to medications like tetracycline or fluoride.
b) Formed over some time.
Two of the most common causes of gradually forming tooth discoloration are: 1) The natural darkening process associated with aging or 2) Persistent exposure to chromogenic agents (coffee, colas, tobacco products, etc…).
For individual teeth, causes can include tooth decay, issues associated with existing dental restorations, or changes that have occurred inside the tooth (in response to nerve injury or death, or as a result of having had root canal treatment).
c) Formed recently.
Discoloration that’s formed just recently (days, weeks, a few months) is frequently due to the accumulation of tooth surface staining. This is the type of debris that a dental cleaning should be able to remove.
Sudden discoloration of isolated teeth may be due to recent tooth trauma.
II) What portion of each tooth is affected? –
a) The whole tooth.
Does the discoloration involve –
1) All teeth.
The cause of the staining may be age-related, due to exposure to chromogenic agents (coffee, tobacco, etc…), or genetic factors.
Prolonged systemic exposure to medications (such as tetracycline or fluoride) during tooth development may also result in whole-tooth staining. In some cases, the formation of surface staining (due to poor oral hygiene) may be the cause.
2) Just some teeth.
When just isolated teeth are affected, look for causes such as a history of tooth trauma or root canal treatment. Other possible causes can include extensive tooth decay, factors associated with a large existing filling, or the formation of surface stains on individual teeth that are difficult to clean.
b) The discoloration is just spots, lines, or patches.
Does the discoloration involve –
1) All or most teeth.
When just isolated areas of many teeth are affected, a common cause of staining can be repeated systemic exposure to medications (such as tetracycline or fluoride) during tooth development.
In cases where dental plaque is not controlled, the formation of white spot lesions (an early form of tooth decay) may be the cause.
2) Just one or a few teeth.
When isolated areas of just one or a couple of teeth have discolored, look for causes such as tooth decay, a stained or deteriorated dental filling, or surface staining due to lax oral home care.
III) Has the tooth’s surface been affected?
Yes –
Severe cases of fluorosis can involve surface pitting. Tooth decay and/or deteriorated dental fillings can result in surface roughness or voids.
Genetic conditions may affect tooth color, shape & formation, or surface texture. Dental tartar accumulation may encrust a tooth’s surface.
Page references sources:
Sánchez AR. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity.
Walsh M, et al. Dental hygiene: Theory and practice. Chapter: Oral hygiene assessment: Soft and hard deposits.
All reference sources for topic Tray-based Teeth Whitening.