Wisdom tooth complications – Gum disease (periodontitis).
If you’re reading this page, you’ve probably been advised that you have a wisdom tooth that should be extracted. And one of the justifications for this recommendation involves issues associated with the presence (or anticipation) of periodontal disease.
Gum disease certainly can be a very valid reason to extract third molars. And as a preview of what you’ll find explained on this page, here are some common guidelines.
Should a wisdom tooth with gum disease be treated or extracted?
Factors that favor extraction.
- The tooth has advanced gum disease.
- Difficult access and/or a challenging root anatomy makes the outlook for treatment poor.
- The tooth holds little dental importance (like in regard to function or future treatment planning).
- The 3rd molar’s gum-health issues place the adjacent 2nd molar at risk.
- It seems doubtful that the patient can adequately maintain (brush and floss) the tooth over the long-term.
- The patient prefers extraction to having periodontal treatment.
Print out for discussion with your dentist.
The remainder of this page explains these issues in greater detail.
Maintaining gum health with wisdom teeth can be difficult.
Third molars can be a challenge to clean. And in cases where they are, they run a greater risk of developing periodontal problems (gum disease).
This is an important issue because the health of the gum tissue surrounding your 3rd molars doesn’t just affect them alone but potentially other teeth in your mouth as well. And for this reason, the removal of your wisdom teeth may be a needed preventive measure.
1) Why are some wisdom teeth at increased risk of developing periodontal problems?
Background.
Gum disease is caused by oral bacteria. And whenever a tooth can’t be cleaned properly on a regular basis, the bacterial-laden film (dental plaque) that accumulates around it may lead to its formation.
The added problem that third molars can pose.
The positioning of some wisdom teeth can be such that it makes them exceptionally difficult (if not entirely impossible) to clean.
And when this type of added challenge exists, these teeth are at even greater risk for developing a periodontal (gum tissue) condition (either just minor [i.e. gingivitis] or advanced [i.e. periodontitis]).
Cleaning challenges unique to wisdom teeth.
a) Tooth impaction.
Plaque that accumulates in the space under the gums can’t be removed.
That scenario makes the perfect recipe for the development of gum disease around the tooth.
b) Gum tissue flaps.
Some wisdom teeth have a flap of gum tissue that lies over their chewing surface. This “lid” overlying the tooth is referred to as an operculum (see picture).
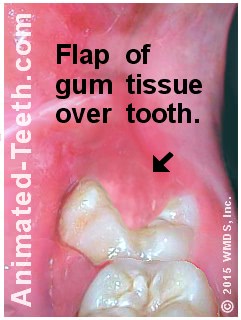
The extra flap of gum tissue on this tooth makes it impossible to clean.
Notes:
When so, this condition can exist simply because there isn’t enough length in the jawbone to accommodate both the tooth and normal gum tissue contours.
The difficulty.
c) Difficult access.
No matter what their orientation in the jawbone is, a general problem that all wisdom teeth share is that by nature they occupy a position in the rear of the mouth that is simply difficult to access with a toothbrush and floss.
That means, even fully erupted, normally positioned wisdom teeth can be extremely challenging to keep clean. And for that reason, they may be at elevated risk for developing gum disease.
2) The gum disease around a tooth is not an isolated event.
The conundrum.
For many dental patients, the following statements about the need to extract their wisdom teeth may seem a little confusing. It’s common that …
- A dentist will suggest removing a wisdom tooth so it doesn’t develop advanced periodontal disease (periodontitis).
- But if the tooth isn’t extracted and ultimately does develop significant gum problems, the treatment recommended at that time will probably be the same, pull it.
With either scenario, you end up losing the tooth. So it’s easy enough to see why a patient might think why not just wait to see if any problems (tooth looseness, pain, swelling) actually occur.
◄ Rear of mouth. | Front of mouth. ►
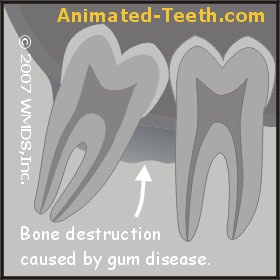
Gum disease damage can impact both the 2nd and 3rd molars.
The 2nd molar may be affected too.
So, if damage occurs (characteristics of advanced gum disease [periodontitis] include bone destruction and gum recession), two teeth are actually affected not just one. (See illustration.)
Additional issues with the 2nd and 3rd molar relationship.
Wisdom teeth are noted for the diverse range of orientations they may have. Pictures. And in some cases, the positioning/angulation of a third may be such that the amount of bone that exists between it and the 2nd molar is comparatively thin.
▲ Section references – Koerner, Hupp
Possible symptoms.
Associated with the patient’s developing condition will be chronic gum tissue inflammation, evidenced by gum tenderness, redness and bleeding that’s easily provoked.
As the patient’s condition worsens, the wisdom tooth might become noticeably loose (as more and more bone is lost), and acute episodes may be experienced from time to time (flareups involving pain and swelling) during periods when the infection that’s present enters an especially active phase.
Outcomes –
For the wisdom tooth.
As mentioned above, tooth extraction is a common treatment solution for cases of advanced gum disease involving third molars.
While other treatment approaches are possible, the successful outcome of this therapy can be hard to predict. That’s both from the standpoint of:
- The dentist having to perform the work for a difficult location. (Access can be difficult, the dental anatomy of this region can pose challenges.)
- And the patient having the skills and motivation to regularly and adequately clean the tooth. (A factor that’s needed for long-term success.)
For the 2nd molar.
In cases where extensive bone destruction has occurred, there may be no realistic alternative other than extracting both the 3rd molar and 2nd molar too. However, it would be the hope that treatment can provide a solution by which the tooth can be salvaged. Obviously, case specifics and the patient’s wishes will be the deciding factors.
What we can state is that most people would sorely miss a second molar. And it would be a shame to lose or have one of these valuable teeth compromised simply because a wisdom tooth that was identified as not being possible to properly cleanse was not extracted before problems developed.
Other 2nd molar concerns.
It’s not just gum disease that can damage the second molar in this type of situation. Tooth decay may play a role too.
The bone destruction associated with periodontal disease can result in spacing between teeth that trap food, plaque and debris. This mixture can create the perfect environment for the formation of tooth decay. Detecting cavities with x-rays. If it does and it’s not caught soon enough, the teeth involved may be damaged beyond repair.
[Experiencing problems with cavities Diagrams | Pictures is another one of the “Valid reasons to extract wisdom teeth” issues that we discuss on our pages.]
3) How likely is it that your wisdom tooth will encounter problems with gum disease?
Incidence rates.
- An evaluation of dental literature (Pogrel) concluded that the incidence rate of experiencing periodontal complications with a wisdom tooth runs on the order of 1% to 4.5%.
- This paper also stated that dental patients over the age of 25 years were roughly twice as likely to have an asymptomatic periodontal defect associated with a third molar, as compared to younger patients.
– The term asymptomatic means “showing no symptoms.” So in these cases, a gum problem existed even though the patients were unaware of them.
– Additionally, this finding simply documents what dentists already know. Older people tend to have more problems with gum disease than younger ones. So, in the case where you are comparatively young and some type of marginal problem already exists with your tooth. Going ahead and having it removed may make preventive sense.
Correlations.
Here are some of the correlations research studies have found.
- a) Two large scale studies found that there’s a greater probability of finding deep (5mm and greater) periodontal pockets on the distal of 2nd molars (the in-between space identified in our picture) when a visible wisdom tooth is present.
– The term “visible wisdom tooth” precisely describes the two difficult to clean situations we explain above: 1) An erupted wisdom tooth that’s simply hard to access or 2) A partially erupted one, which often involves the situation where almost no below-the-gum-line cleaning can be accomplished at all. In either case, you would expect periodontal problems to exist.
- b) Other studies have shown that having a visible 3rd molar correlates with the subject’s overall level of periodontal disease severity.
– This finding simply reinforces the fact that gum disease is not a localized event. It tends to affect other areas of the mouth as well.
- c) Some studies have focused on the types of bacteria living below the gum line around wisdom teeth and the level of pathologic periodontal activity taking place in that person’s mouth.
– The idea associated with these findings is that non-maintainable areas around wisdom teeth can harbor the types of bacteria known to be the causative agents of gum disease. And their presence there tends to impact the health of the mouth as a whole.
▲ Section references – Pogrel
4) If gum disease is found around wisdom teeth, what should be done?
No one can debate that it can be extremely difficult, if not impossible, for a person to effectively remove dental plaque from around their third molars. But what is debatable is exactly how this difficulty should be managed.
Should the teeth be removed?
Obviously, you’ll have to rely on your dentist’s judgment. Extraction is one solution but it’s not always required.
Non-extraction approaches.
If the bacterial infection (gum disease) surrounding your wisdom teeth can be brought under control and subsequently managed, then there’s no real reason to remove them. This might be accomplished via one of the following approaches.
- More effective oral home care (better brushing and flossing How to. | Dos & don’ts., and possibly incorporating the use of an electric toothbrush Top brands. into your cleaning routine).
- More frequent or extensive dental cleanings (scaling and root planing).
- The use of gum surgery to improve the tooth-gum relationship so adequate cleaning is possible.
Obviously, only your dentist can counsel you on which approach, extraction or alternative, seems to offer the most appropriate solution for your situation.
In the case where the teeth are retained, the level of home care you perform on a daily basis will likely be the deciding factor in what your long-term outcome will be. If you can’t commit to keeping that level high, extraction may make the more realistic choice.
Page references sources:
Hupp J, et al. Contemporary Oral and Maxillofacial Surgery. Chapter: Principles of Management of Impacted Teeth.
Koerner KR. Manual of Minor Oral Surgery for the General Dentist. Chapter: Surgical Management of Impacted Third Molar Teeth.
Pogrel MA, et al. American Association of Oral and Maxillofacial Surgeons White Paper on Third Molar Data.
All reference sources for topic Wisdom Teeth.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Unable to do bone graft after extraction due to infection
I am 62 and have had periodontal disease for years. Have had several s&rp, a surgery 20 years ago, etc… and periodontal maintenance appt every 2 months.
All wisdom teeth impacted and never removed. Biggest problem area is last tooth upper right with deep pockets and frequent “flares” between appt. During this year, flares worse with roof of mouth swollen and painful, not just gum around tooth.
My dentist retired and dentist that took over practice (who specializes in implants) evaluated my situation. There is already bone loss. He recommended only pulling last tooth and doing bone graft and NOT doing implant. He thought adjacent tooth was ok, if we did it now. Procedure scheduled for 2 weeks. But another flare. So ordered amoxicillin and push up extraction for day 5 of 10 day amoxicillin. Unfortunately, he said there was way too much infection to do the bone graft… I go back in a month, but he said the graft probably isn’t an option since we didn’t do it immediately after the extraction. Would it be beneficial to do graft if not done at the time of extraction but some later time?
Carol
Reply –
Carol, your question really lies far beyond what any comments section of a website could provide a qualified answer to.
As background, what may be an issue is that after a tooth has been extracted, bone height and width in that area is lost. (This is a normal part of the post-extraction bone healing process.)
Placing grafting materials at the time of extraction can help to prevent how much bone loss occurs (this would be referred to as performing a “ridge preservation” procedure).
In your case, due to the complications that occurred, a normal/usual amount of bone loss will occur and this may result in a situation that is less ideal for grafting (their recommendation for the graft was predicated on them having the previous amount/configuration of bone to work with).
Only your dentist can determine (after examining you and taking x-rays) if grafting at this later date makes a suitable plan. While you may be eager to have done whatever can be done, your dentist (the person who knows the facts of your case) has a responsibility to you to only suggest treatments that have a reasonable chance of providing a benefit for you. That may be why they haven’t made the recommendation.
Staff Dentist