Dental paresthesia: Nerve damage as a complication of wisdom tooth extraction or dental injection.
Paresthesia (nerve damage) as a postoperative complication of tooth extraction.
Table of contents –- What is Paresthesia?
- Introduction – Causes, signs, outcomes.
- As a complication of tooth removal – Causes. | Nerves most affected.
- Associated with dental injections – Causes. | Nerves most affected.
- Details about experiencing paresthesia.
- Signs and symptoms – Altered or loss of sensation. Effects on speech and function.
- Risk factors.
- Tooth position – Nerve proximity. | Identifying risks using x-rays.
- Surgical factors and clinician skill.
- Age.
- Factors associated with dental injections.
- Frequency – Incidence rates.
- Recovery.
- Duration of symptoms – Transient, persistent, permanent.
- Signs of recovery.
- Treatment approaches.
- Documenting/mapping the affected area.
- Treatment with medications – OTC and prescription.
- Surgical repair – Timing. | Success rates.
- Other ways to learn.
- This page’s highlights as a video.
- This page’s comments section.
- Introduction – Causes, signs, outcomes.
- As a complication of tooth removal – Causes. | Nerves most affected.
- Associated with dental injections – Causes. | Nerves most affected.
- Signs and symptoms – Altered or loss of sensation. Effects on speech and function.
- Tooth position – Nerve proximity. | Identifying risks using x-rays.
- Surgical factors and clinician skill.
- Age.
- Factors associated with dental injections.
- Frequency – Incidence rates.
- Duration of symptoms – Transient, persistent, permanent.
- Signs of recovery.
- Documenting/mapping the affected area.
- Treatment with medications – OTC and prescription.
- Surgical repair – Timing. | Success rates.
- This page’s highlights as a video.
- This page’s comments section.
What is paresthesia?
Dental paresthesia is a possible postoperative complication associated with the removal of teeth (most frequently lower wisdom teeth), or in some cases receiving a dental injection.
(This condition can also be a post-op complication associated with having root canal treatment or dental implant placement but that is not the focus of our coverage here.)
Causes – The onset of paresthesia is a result of nerve trauma. It involves the situation where during the patient’s procedure a nerve lying in the immediate area has received some type of insult.
In most cases, the event involved has crushed, bruised, stretched, or otherwise irritated the nerve. Less likely, it may have actually been nicked or severed.
Signs and Symptoms – As a result of the nerve injury, the person experiences a change in, or loss of, sensation in the tissues and structures that are serviced by the nerve. The lip, facial skin, tongue, and lining of the mouth are all commonly affected areas.
Outcomes – The altered state typically persists for an extended period (days, weeks, months), ultimately resolving on its own without specific treatment. In some cases, the change in sensation that’s noticed may be permanent, or only partially resolves.
This page’s highlights as a video –
Subscribe to our YouTube channel.
Details.
As mentioned above, dental paresthesia may be a complication associated with tooth extraction or receiving a dental injection. We discuss each situation separately:
a) Paresthesia as a complication of tooth removal.
Most cases of paresthesia following an extraction occur in conjunction with the removal of lower third molars (wisdom teeth) and to a lesser extent lower second molars (the next tooth forward).
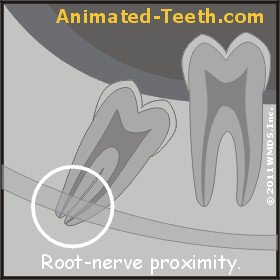
Tooth roots lying in close proximity to the Inferior Alveolar nerve.
Which nerves are usually affected?
The major nerves that lie in close proximity to 2nd and 3rd molars (wisdom teeth), and thus are at risk for receiving trauma or damage during the extraction process, are:
- The Inferior Alveolar nerve. – This nerve runs the length of the lower jawbone in its Mandibular canal (a tunnel-like structure through which the nerve and associated blood vessels run).
The canal lies more or less in the center of the jawbone, at a level lying just below the roots of the teeth it holds (when they are fully erupted, thus explaining why the roots of impacted teeth tend to lie close to this nerve, see illustration above).
At a point near its end, the Inferior Alveolar nerve gives rise to a branch called the Mental nerve. It exits the jawbone and runs to and services the tissues of the lower lip and chin region. (If the Inferior Alveolar nerve displays symptoms of paresthesia, this branch will too.)
- The lingual nerve. – This nerve runs through the soft tissues that cover over the inside surface of the lower jaw. It provides services for these tissues, and also branches off to and provides sensory perception for the tongue.
What can cause nerve injury that leads to paresthesia?
Nerve bruising or stretching can result in significant levels of nerve irritation. Compressive forces may physically crush the nerve. Less likely, the nerve may have been partially or even completely severed.
- Compressive forces might be generated by the movement of the tooth as it’s loosened up or removed, or by the extraction instruments being used. (An explanation of how teeth are removed. Extraction techniques.)
- The dental drill or hand instruments used to remove bone tissue or section the tooth Surgical extraction techniques. during the extraction process may nick or sever the nerve.
- To gain access to the tooth, a gum tissue flap Soft tissue techniques. may need to be created. During events associated with incising and/or retracting this tissue, the nerve that lies within it may be traumatized or even severed.
b) Paresthesia associated with dental injections.
Other than surgical procedures, some cases of paresthesia are caused by routine dental injections (administering local anesthesia, getting a dental “shot”).
Which nerves are most often affected?
The greatest risk of paresthesia lies with injections given in the back of the mouth to numb up lower teeth. This is termed an inferior alveolar nerve block injection. Kinds of dental injections.
- The Lingual nerve. – This is the same nerve mentioned above that runs through the soft tissues that cover the inside surface of the lower jawbone. 70% of cases involve the Lingual nerve.
- The Inferior Alveolar nerve. – This is the nerve mentioned above that runs through the jawbone’s Mandibular canal. However, as related to injection paresthesia, the location at which the nerve is traumatized is before its enters the bone (at a point during which it courses across the inside surface of the posterior jawbone).
- The Maxillary nerve. – While rare, this nerve that services aspects of the upper jaw may be affected.
Two of the branches of the Trigeminal cranial nerve are the Maxillary and Mandibular nerves. The Inferior Alveolar and Lingual nerves are branches of the Mandibular nerve.
What creates injection nerve trauma?
The irritation or damage caused may be due to one or a combination of the following:
- Direct trauma caused by the needle itself.
The largest gauge needle used in dentistry has a diameter of .45mm. In comparison, the size of the nerves that lie at risk is on the order of 4 to 7 times larger (on the order of the size of a spaghetti noodle).
For this reason, a nerve receiving a nick is the most likely event, as opposed to being severed completely.
- Hydrostatic pressure.
The process of injecting a local anesthetic into soft tissue may result in the creation of pressure that compresses/traumatizes adjacent nerve fibers.
- Hematoma formation.
The movement of a needle through soft tissues may rupture blood vessels, thus causing the release of blood. Constriction of the hematoma (swelling of clotted blood) that then forms may place pressure on nerve fibers that pass through it.
- Neurotoxicity of the anesthetic. – The nature of the anesthetic used may cause localized chemical damage to the nerve.
Some studies suggest that local anesthetics used in dentistry as more concentrated solutions (such as 4% prilocaine or 4% articaine) are more frequently associated with the development of paresthesia than lower-concentration formulations (such as 2% lidocaine).
▲ Section references – Garisto
Signs and symptoms of paresthesia.
In most cases, the nerve injury that has occurred is not identified during the dental procedure itself but instead by way of symptoms that appear during the hours that follow the wisdom tooth removal, extraction, or injection.
Paresthesia – Signs and symptoms.
- The person experiences an altered, diminished, or even total loss of sensation.
While on this page we tend to use the word “paresthesia” as an all-encompassing term, most precisely it refers to experiencing abnormal sensations. This might include tingling, numbness, or a “pins and needles” effect (similar to the feeling a person experiences when they have a tooth anesthetized for a dental procedure).
In comparison, a diminished sense of feeling is termed “hypoesthesia.” The total loss of sensation is referred to as “anesthesia.” Some people experience “dysesthesia,” the feeling of painful or unpleasant sensations.
- The location and extent of the affected area reveal which nerve(s) has been affected.
Damage to the Inferior Alveolar nerve will cause sensation changes in the lower lip and chin. Injury to the Lingual nerve will affect sensations in the tissue lining the inside of the jaw and also the tongue.
- One or more sensations may be affected: touch, pain, proprioception, temperature, or taste.
A person will feel an altered, reduced, or even total loss of sensation in the affected area. Patients frequently report experiencing a sensation similar to the numbness they feel when being numbed up for a dental procedure (tissue “tingling”). Additionally, any combination of senses may also be affected including loss of taste, touch, or temperature perception.
- The effects may affect/alter/inhibit many kinds of activities, such as speech, chewing, playing a musical instrument, cause drooling, etc…
Even when the effects experienced are just minor, they can be difficult for a person to cope with. Their quality of life may be significantly affected. Social interactions may be inhibited.
Other characteristics.
- It’s important to note that paresthesia is a sensory-only phenomenon. That means its symptoms do not involve muscle function issues like paralysis, spasms, or loss of control. Some activities (eating, speaking, etc..) may be altered or inhibited by the person’s loss of sensation but these changes are not due to loss of muscle function.
Characteristics unique to dental injection paresthesia.
On occasion, while receiving a dental injection a person may experience an “electrical shock” sensation as the needle makes physical contact with their nerve. (This would be most common with inferior alveolar nerve block injections, the type of “shot” used to numb up lower back teeth.)
Having experienced a shock is not necessarily an indication that paresthesia will occur but there is a relationship.
- As many as 15% of people who experience this sensation go on to experience some degree of paresthesia.
- 57% of people who ultimately do experience paresthesia did experience the shock effect.
▲ Section references – Smith
How long does the numbness/sensory loss of paresthesia last?
For those patients who are affected, one of 3 scenarios will play out.
- In most cases, the paresthesia is transient, resolving on its own after a short period, usually measured in one or two to several weeks.
- With cases lasting longer than 6 months, the condition is classified as being persistent.
- For a small number of cases, the loss (complete, partial, or partially resolved) is permanent.
We discuss statistics and events associated with case progress and outcomes in greater detail below.
Evaluating a patient’s risk for paresthesia.
A) Location, location, location.
As discussed above, one primary risk factor for paresthesia is simply the proximity of the tooth being extracted to nearby nerves (and therefore increased likelihood that they’ll be traumatized during the extraction process).
Identifying risk using x-rays.
2-D vs. 3-D imaging
One difficulty associated with using x-rays to make this determination is that common dental radiographs are just a 2-dimensional representation (a flat picture) of a 3-dimensional configuration. And for this reason, only an educated guess can be made about the precise relationship that exists.
A more definitive determination can be made using the cross-sectional imaging possible with 3-D radiography, such as a Cone Beam CT scan. This technology is becoming more and more commonplace in the offices of oral surgeons, and even some general practitioners too.
It does however come at a greater expense, both in financial terms and in the level of radiation the patient is exposed to.
Is 3-D x-ray imaging really necessary?
Only the dentist performing the patient’s work can determine if this level of evaluation (and the added expense and radiation exposure it involves for the patient) is indicated.
We can report that studies (Deshpande, Kositbowornchai) have determined that traditional 2-D imaging can reliably provide a practitioner with a high level of information regarding the configuration that exists, especially when a multi-x-ray technique is used. But of course, it is not as definitive as 3-D imaging.
▲ Section references – Deshpande, Kositbowornchai
Checklist – Factors that may place your extraction case at increased risk for paresthesia.
- Pre-op exam. – Has the tooth been adequately evaluated? Is 3D x-ray imaging needed?
- Tooth proximity to the nerve bundle. – What relationship and potential risk do x-rays show?
- Tooth positioning. – Impacted vs. erupted. / Impaction type.
- Treatment planning. – Would performing a planned ‘surgical’ extraction lower risks?
- Clinician skill and experience. – General dentist vs. referral to an oral surgeon.
- Local anesthetic. – Type of injection, anesthetic used.
- Patient factors. – Age / Completeness of root formation.
Print out and add notes to discuss with your dentist.
Risk according to impaction type.
- Any lower wisdom tooth that’s angled or positioned toward the tongue side of the jawbone places the lingual nerve at greater risk.
- Lower full-bony impactions, especially horizontal and mesio-angular ones Impaction types: Diagrams, are the type of extraction most likely to result in trauma to the mandibular nerve.
B) Surgical factors.
Clinician skill.
A research paper by Jerjes bluntly states that one of the main risks for developing permanent sensory loss as a complication of nerve damage experienced during tooth extraction was the surgical skills/experience of the operator.
▲ Section references – Jerjes, La Monaca
Oral surgeon vs. general dentist.
There are a number of procedural steps that can help prevent nerve damage from occurring during lower wisdom tooth extractions. They include:
- Appropriate gum flap design, and careful manipulation. Minimizing the amount of bone removed from the back and tongue sides of the tooth. Sectioning the tooth into parts for easier removal. Making sure the path of tooth removal (as related to the curvature of its roots) is appropriate. Careful and appropriate socket debridement after the tooth has been removed. (La Monaca)
▲ Section references – Jerjes, La Monaca
C) Age as a risk factor.
This is one reason why asymptomatic full-bony impacted wisdom teeth that show no sign of associated pathology are often left alone in people over the age of 35.
C) Dental injections.
The vast majority of cases of paresthesia resulting from dental “shots” involve those used to numb up lower back teeth (specifically inferior alveolar nerve blocks).
But as opposed to oral surgery where the patient’s risk can be evaluated during their procedure’s planning stage, there’s no way for a dentist to anticipate beforehand which dental injections might result in this complication.
Paresthesia occurrence – Statistics.
a) As related to wisdom tooth extraction.
In a review of research studies that evaluated symptoms of nerve damage after wisdom teeth removal, Blondeau found incident rates for paresthesia ranging from 0.4% and 8.4%.
One large study (Haug) evaluated the outcome of over 8,000 third molar extractions. It found an incidence rate of less than 2% for subjects ageed 25 years and older (as mentioned above, an age group that’s relatively at risk for this complication).
b) As related to dental injections.
It’s been estimated that roughly 1 out of 27,000 Inferior Alveolar Mandibular blocks (the type of dental injection used to numb up lower back teeth, and the one most associated with this complication) will result in paresthesia.
▲ Section references – Blondeau, Haug, Smith
How long does paresthesia last?
In most cases, a patient’s paresthesia will resolve on its own over time, with the amount of time ranging from just a few days, to several months, to over a year. In some cases a person’s sensory loss, complete or partial, is permanent.
General guidelines about dental paresthesia recovery.
A person’s level of sensory loss, their potential for recovery (full or partial), and the timeline associated with it will all correlate with the type (nerve irritation, crushing, nicking, or severing) and extent of the original injury. Unfortunately, these are factors that are usually unknown.
Experiencing altered or diminished sensation implies that the nerve is still at least partially intact, a situation that favors recovery. But the complete loss of sensation doesn’t necessarily mean that the nerve has been completely severed. A nerve that’s been crushed can display this same symptom.
a) As related to wisdom tooth extraction.
Spontaneous recovery.
In cases associated with lower wisdom tooth removal, Queral-Godoy found that the highest rate of recovery took place during the first 3 months. At 6 months, one-half of all of those affected experienced a full recovery.
Persistent paresthesia.
(This classification refers to cases where the patient’s condition lasts longer than 6 months.)
Pogrel reviewed studies that evaluated symptoms of nerve damage after wisdom teeth removal and found reported incidence rates of persistent paresthesia ranging between 0% and 0.9% for the Inferior Alveolar nerve, and 0% and 0.5% for the Lingual nerve.
Paresthesia recovery – General rules of thumb.
- If a patient’s condition has not completely resolved within a two-month time frame, the probability of their having some degree of permanent sensory deficit increases (although full resolution may still occur).
- If some level of deficit still remains after nine months, it’s unlikely that complete resolution will occur.
▲ Section references – Queral-Godoy, Pogrel, Bhat
b) As related to dental injections.
Spontaneous recovery.
In 85 to 94% of cases, spontaneous complete recovery typically occurs within 8 weeks.
Persistent paresthesia.
▲ Section references – Smith
What to expect with paresthesia recovery.
- Any improvement is a positive sign.
- Progress toward recovery can begin early or later on.
- Early improvement hints at a more complete recovery.
- Even slow / delayed recovery may still be complete.
- Expect the healing process to be gradual.
- The recovery rate of different senses can vary.
- Returning senses tend to sharpen up over time.
- Just partial or even no recovery may be a fact of life.
What can be expected during recovery?
Signs of paresthesia resolution.
Recovery from paresthesia, just like with any type of healing, is a process. And for that reason, any progress toward returning to normal can be expected to be a gradual transformation over a period of time. However, as the statistics above indicate, the time frame involved can be quite variable, ranging from just days to many months, to over a year.
- As sensation in the area starts to reappear, the degree of detail it provides should sharpen over time, hopefully returning all of the way back to normal parameters.
- Since the nerve fibers that transmit different types of sensations have different structural characteristics, one type of sensation may make a quicker recovery than others. As examples, perceptions involving pain and temperature typically appear first (Strauss).
- As you might expect, the sooner the first signs of renewed sensation appear, the more favorable the chances are for complete recovery (see statistics above).
- It may be that no progress is experienced for a period of time (weeks, months), and then signs start to appear.
▲ Section references – Strauss
Why paresthesia recovery rates vary.
The most important determining factor in a person’s rate of recovery (and also how complete their recovery will be) is the nature and extent of the insult/damage that the nerve has received. As simple examples:
Factors that will affect dental paresthesia recovery.
- A nerve that is still structurally intact (like those that have been bruised, stretched, or compressed) can be expected to make a quicker, fuller recovery than one that has been severed.
- Nerves that have been nicked, as opposed to completely severed, have a quicker, more favorable prognosis.
- What’s generally referred to as a nerve is actually a bundle of individual nerve fibers. And as such, some fibers may have received a different type or extent of trauma due to their location in the bundle.
(Following on with the examples above, bruised fibers would be more likely to make a quicker, more complete recovery than those that had been outright severed.)
Of course, in most cases, the nature and extent of what’s occurred isn’t known. And as such, developing any specific rules about patient recovery rates are simply impossible to make.
Checklist of steps to take with post-extraction paresthesia.
- Let your dentist know.
- Arrange for their “mapping” the affected area.
- Mapping provides a baseline for monitoring improvement and identifies the nerve(s) involved.
- Ask what re-evaluation interval they suggest.
- Ask if the use of anti-inflammatory medication is indicated.
- Ask under what scenario consultation about surgical repair might be considered.
- Keep your dentist updated about your status.
- Remain positive. Most cases resolve on their own.
Print out and add notes to discuss with your dentist.
Treating permanent paresthesia.
a) Testing and mapping – Establishing a baseline for comparison.
Testing / mapping the affected areas.
Tests that should be included when evaluating a person’s dental paresthesia.
- Light touch response. – A small cotton ball is brushed against the skin to see if it can be felt and if the patient can discern the direction of the ball’s movement. Moist tissues (like the lining of the mouth) can be difficult to evaluate with this test.
- Sharp vs. dull discrimination. – Areas are prodded with a pin or other sharp-pointed tool. The patient is asked if they can feel a sensation, and if so whether it feels sharp or dull. A comparison to the same location on the patient’s unaffected side is made also.
- Two-point discrimination. – A pair of calipers having a pair of sharp points is systematically touched to the affected area, using various distance settings. The patient is asked if they are able to feel this contact as one or two individual points.
- Taste stimulation. – Cotton balls soaked in saline (salt), sugar (sweet), vinegar (sour), or quinine (bitter) solution are drawn across the side of the tongue to see if a taste response is triggered.
How often should re-evaluation of dental paresthesia patients be performed?
After the results of a person’s initial testing have been documented, comparisons can then be made periodically to evaluate the patient’s progress toward returning to normal.
▲ Section references – Smith
b) Treatment with medications.
The use of some types of drugs may be beneficial in the management of nerve-related injuries. But there doesn’t seem to be a widespread consensus or recommendation in published dental literature regarding the specific medications or regimens used with dental paresthesia.
Considering that most cases of paresthesia resolve on their own, possibly practitioners don’t feel, or understand, a need for additional treatment therapies. Some of those mentioned in dental literature involve:
Anti-inflammatory medications.
The idea associated with the use of anti-inflammatory drugs is that they can help limit the level of inflammation that occurs in association with the traumatized (stretched, bruised, compressed, etc…) nerve that might impede its recovery process. (Like nerve fiber or associated tissue swelling, disruption of the nerve’s associated microcirculation, etc…)
Two different classes of drugs might be chosen for this purpose. In some cases, they might be used in conjunction with each other.
Classes of anti-inflammatory medications sometimes used in treating dental paresthesia.
- Steroids – Examples include oral dexamethasone or prednisolone.
- NSAIDS (nonsteroidal anti-inflammatory drugs) – An example would be ibuprofen/Motrin.
▲ Section references – Juodzbalys
An example of using ibuprofen (Motrin) as an aid in the resolution of dental paresthesia.
A paper by Juodzbalys mentions a regimen of 800mg of ibuprofen 3 times daily for 3 weeks as a treatment assisting with the recovery of paresthesia resulting from dental implant placement.
Even in cases where the patient’s doctor deems this approach appropriate, and the medication is appropriate for the patient’s use, side effects such as gastric irritation and ulcer formation may occur, especially with long-term use.
Additional benefits.
Some cases of paresthesia (especially those caused by dental injection) may be due to pressure/compression directed on the nerve by local swelling. If so, an anti-inflammatory approach would assist in controlling this etiology.
Adrenocorticosteroids.
The use of adrenocorticosteroids (a type of steroid compound produced by the human body) early on after the patient’s injury may help to minimize some types of neuropathy from forming during the healing process, thus promoting a more favorable outcome. (Juodzbalys)
c) Surgical repair. / Microsurgery.
In cases of persistent or permanent paresthesia, surgical repair may be possible.
Potential candidates.
It’s clearly best stated that a decision to attempt a repair, and subsequently the timing for it, depends on the nature of the sensory change experienced (full or partial loss, painful, recovering, etc…) and is therefore best evaluated by the doctor (oral-maxillofacial surgeon, neurosurgeon or micro-neurosurgeon) who will provide the treatment.
As general guidelines …
Potential candidates for surgical repair of paresthesia:
- Patients who experience anesthesia (complete loss of sensation) for 2 to 3 months with no improvement.
- Patients who experience paresthesia (altered sensation) for 4 to 6 months with no improvement for 2 months.
- Patients who experience dysesthesias (painful or uncomfortable sensations) for a minimum duration of 2 to 3 months.
▲ Section references – Juodzbalys
Timing.
Once again, it will be the nature of the patient’s case that will determine when a repair might be best attempted. And that decision is best made by the doctor who will be performing the surgery.
As you’ll see below, the possible timing for secondary repair (surgical repair made after the date of the patient’s original injury) can vary widely, and it may affect the procedure’s outcome. That suggests to us that the potential need for surgical repair should be discussed relatively early during the healing process so no window of opportunity that might have been an asset is lost.
Selected time frames for surgical repair of paresthesia.
- Surgery may be delayed until a point 6 to 12 months after the original injury, so to allow the healing process to continue to the point of its completion (no further improvement) before a decision is made.
- Some studies (see below) seem to have found that prompt repair increases the chances of case success. And, in fact, it may be that the most favorable window for an attempted (secondary) repair lies at about three months after the original injury. (Juodzbalys)
- It may be that in situations where it is positively known (visualized) or highly suspected that the nerve has been severed that proceeding promptly with a repair provides the most favorable outlook.
- Despite what in hindsight might have been considered ideal for a patient’s case, attempts made at a later time are thought to be capable of yielding reasonable results.
(Notice that some of the studies we cite below report surgeries having been performed multiple years following the patient’s original injury. We don’t, however, know the outcome of these specific cases.)
Paresthesia repair – Microsurgery success rates.
A paper by Pogrel reports that results for surgical intervention vary widely. Success rates appear to range between 50 and 92%, however, some reported successes only involve partial recovery. Even if just partial recovery was achieved, many patients still considered the attempt worthwhile.
A sampling of findings reported by research studies:
- Strauss evaluated the outcomes of Inferior Alveolar nerve repair experienced by 28 patients treated by one surgeon.
50% reported significant improvement in their condition, 43% slight improvement and 7% gained no benefit. The average wait period before a surgical repair was attempted was 6.6 months following the patient’s initial injury.
- Bagheri evaluated the outcome of 186 Inferior Alveolar nerve repair surgeries performed by multiple surgeons. On average the surgeries were performed 10.7 months following the patient’s initial injury, with the range being 0 to 72 months).
It was determined that 81% of cases resolved favorably, resulting in either a functionally useful (partial) or complete recovery. The study noted a drop in case success for surgeries performed at a point 12 months and beyond the patient’s initial injury.
- In an evaluation of 222 Lingual nerve microsurgeries performed by multiple surgeons, Bagheri reported 66% of cases experienced complete recovery, 25% functionally useful recovery, and the remainder had no or inadequate improvement.
On average, the surgeries were performed 8.5 months after the patient’s initial injury (range 1.5 to 96 months). The study noted that shorter intervals tended to improve case outcomes. It also found a significant drop in case success for surgeries performed at a point 9 months and beyond the patient’s initial injury.
▲ Section references – Bagheri, Joudzbalys, Pogrel, Strauss
Page references sources:
Bagheri SC, et al. Retrospective review of microsurgical repair of 222 lingual nerve injuries.
Bhat P, et al. Inferior Alveolar Nerve Deficits and Recovery Following Surgical Removal of Impacted Mandibular Third Molars.
Blondeau F, et al. Extraction of impacted mandibular third molars: postoperative complications and their risk factors.
Deshpande P, et al. Proximity of Impacted Mandibular Third Molars to the Inferior Alveolar Canal and Its Radiographic Predictors: A Panoramic Radiographic Study.
Garisto GA, et al. Occurrence of paresthesia after dental local anesthetic administration in the United States.
Haug R, et al. The American Association of Oral and Maxillofacial Surgeons Age-Related Third Molar Study.
Jerjes W, et al. Risk factors associated with injury to the inferior alveolar and lingual nerves following third molar surgery-revisited.
Juodzbalys G, et al. Injury of the Inferior Alveolar Nerve during Implant Placement: a Literature Review.
Kositbowornchai S, et al. Ability of two radiographic methods to identify the closeness between the mandibular third molar root and the inferior alveolar canal: a pilot study.
La Monaca G, et al. Prevention of neurological injuries during mandibular third molar surgery: technical notes.
Pogrel MA, et al. American Association of Oral and Maxillofacial Surgeons White Paper on Third Molar Data.
Queral-Godoy E, et al. Incidence and evolution of inferior alveolar nerve lesions following lower third molar extraction.
Smith M, et al. Nerve injuries after Dental Injection: A review of the literature.
Strauss ER, et al. Outcome assessment of inferior alveolar nerve microsurgery: a retrospective review.
All reference sources for topic Wisdom Teeth.
Video transcription.
Hello, and welcome to Animated Teeth.com and our page that discusses the post-operative complication of nerve damage following a tooth extraction. Dentists refer to this condition as paresthesia.
We can only imagine the disappointment a person must feel as they discover this complication has affected them. Fortunately, it’s possible to state that most cases of paresthesia finally do resolve on their own. So, one can only hope that that will be the case for you too.
As you wait and endure, you’ll no doubt have questions about what has transpired to cause your condition, and then, what may happen in the future. This video and its accompanying page should be able to provide that information.
In regard to what has happened, paresthesia occurs as a result of nerve fiber trauma created during the extraction process. And, from that point of damage or irritation, and on towards its end, the tissues serviced by the affected portion of the nerve will experience altered sensation.
The trauma that created your condition can take different forms. For example, the nerve might have received compressive force as pressure was applied to the tooth to loosen it up. If so, this force might have bruised or crushed your nerve.
In comparison, direct damage would be caused if the nerve was nicked or even severed by a dental instrument, like a scalpel. Or, the fiber could be cut, torn, or stretched as a consequence of performing a procedural step, like raising a gum tissue flap, especially in certain risk-prone areas.
It’s even possible that a person’s paresthesia is the result of trauma created during the injection of anesthetic. In this scenario, the trauma might be caused by the needle, the hydrostatic pressure created during the injection process, or even the chemical nature of the anesthetic itself.
With such a wide range of possible causes, you might wonder how frequently this complication occurs. Paresthesia stemming from dental anesthetic injections is considered rare. During their career, a dentist will likely only witness a few cases, if any.
With extractions, most paresthesia cases are associated with removing lower wisdom teeth. Our graphic here shows why. The roots of these buried teeth can have a close association with the nerve bundle that services them, and that places it at risk.
As far as how often this complication occurs with this most likely type of case, study estimates vary but we’ll cite one that suggests that the incidence rate lies on the order of 2% or less.
Additional risk factors include the degree of root formation. About two-thirds is usually ideal for removing impacted teeth. The age of the patient, where comparatively younger people usually fare better. And clinician skill and experience, where, of course, their having more generally helps to lower your risk.
The precise symptoms that an affected person will experience can vary. And to explain how, we need to introduce a few additional terms. The one you already know, paresthesia, is frequently used as the catch-all term for this complication. But more precisely, it really refers to the situation where the affected tissues have abnormal sensations, like tingling or a pins-and-needles effect.
If instead the patient notices a diminished level of sensation in their affected area, the term hypoesthesia is used. The total loss of sensation is called anesthesia. And the word dysesthesia applies to situations where the area produces painful or unpleasant sensations.
Anyone experiencing this complication will be curious about how long their condition may last. A study evaluating lower wisdom tooth cases determined that the highest rate of recovery took place during the first three months. And at six months, one-half of all cases achieved full resolution.
Generally, earlier signs of recovery tend to favor complete resolution. Cases that haven’t resolved after two months may not recover fully, although they may. Cases still showing some sensory deficit after nine months are even less likely to fully resolve.
As far as signs of recovery go, any improvement that’s noticed should be considered a positive. Precisely when improvement first appears varies, so don’t be too disappointed initially. And expect your recovery to be gradual. Also, different senses, like hot and cold versus pain, may return at different times or rates.
At this point in our video, you may have noticed that we haven’t yet discussed how paresthesia is treated. And for the most part, no specific treatment is usually performed. A patient’s recovery relies on their body’s ability to make a repair on its own.
Some dentists do employ the use of anti-inflammatory medications with their patients’ paresthesia cases. And, as this page details, that includes some common over-the-counter ones.
As a related point, we’ll mention that it’s hard to know how much improvement has occurred if the size, shape, and location of the affected area weren’t mapped out initially. So, sensory testing should be performed early on and its results documented. Our page’s text outlines what’s usually done.
For those cases where no or just limited improvement has occurred, especially over the comparatively longer term, an attempt at surgical repair might be indicated. Our page’s text explains what sort of guidelines might be used when deciding.
As a point of advice for those struggling with stubborn cases, keep in mind that many general dentists will only have a limited amount of experience with this condition. In comparison, an oral surgeon whose practice is primarily composed of performing surgical procedures will encounter this complication much more frequently.
Based on their greater familiarity with interpreting case details, and an expectation that they would be more knowledgeable about current trends in treating non-responding cases, a referral for consultation might be considered.
With that point, we’ll conclude this video. Don’t overlook that our accompanying page contains additional information we haven’t discussed. So, give it a read. Also, if you’re suffering with paresthesia, we wish you the best in your recovery. Good luck.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Help!
I had a bottom wisdom tooth pulled and my lip still feels tingly like after having my shots! What do I do? When does this go away?
Drk
Reply –
You haven’t really given us very much information to go by.
We see that your comment is posted on this page, which implies that you think you may have experienced some type of nerve trauma/damage during your procedure.
You also mention that the tooth you had removed was a lower wisdom tooth. A tooth with which the chances of experiencing this complication of are greater.
You don’t state how long you’ve been experiencing the state of altered sensation you’ve noticed. Related to the time of day you posted (late evening, if you’re in the USA), and if you posted on the day of your procedure, it seems it would have been completed many hours previous. If so, yes the anesthetic your dentist gave you would have been expected to have worn off by then.
So, it seems possible that your inferior alveolar nerve did receive trauma during your extraction process and you are now experiencing paresthesia as a result.
From your comment, we don’t really get the impression that you’ve read this page. You should do so. It will help you understand what is going on.
In terms of what to do … the first step is to let your dentist know you are having problems.
They’ll document the extent of your altered senstation, so they can compare that to what’s found during future evaluations.
The good news is that most cases resolve back to normal on their own. However, the bad news is that can take some weeks or months. The information on this page explains everything we just stated in greater detail. Best of luck.
Staff Dentist
Comment –
Paresthesia
May 4 to present June 25. Paresthesia in lip chin is shrinking but still have altered sensations. There is no guarantee of full recovery. Dentist said it was an injection. My second opinion dentist said my tooth implant was compressing the nerve. 2nd molar. Had it removed within a week after surgery
Lisa L
Reply –
Best of luck with this. We hope you continue to show improvement.
Staff Dentist
Reply –
Update.
I spoke to my oral surgeon July 9 I still have altered sensation 2 months later. . We spent 5 minutes talking to each other. He told me I should be completely healed between 6 months and one year and there is no need to make another appointment with him again
Lisa L
Reply –
Update on your progress.
Hello; the exact same thing happened to me this week. I noticed your comment is older: can I have an update on your progress? Did your sensation return? And if not, did your body get used to it at least? I am so scared that I am not going to be able to feel the right side of my face for the rest of my life.
Thank you!
Alex D
Comment –
Damaged Lingual nerve by dentist injection
I had a dental block in the lower right hand side of my mouth for a tiny filing in that lower from tooth. The injection was the longest and most uncomfortable that I have ever experienced and I also experienced a really hectic electric shock sensation, but the dentist did not withdraw the needle, even though he could see I was very uncomfortable.
After about 5 hours, the anaesthetic wore off excepting the right hand side of my tongue and bottom right hand side of the inside if my gums. I called the dentist the next day and he said that it had occurred to another patient of his and it can happen as it is a blind injection and I must keep him updated. I said that I was not happy with that and wanted him to see me and assist me with advice on what couid be done.
I went into see him that same morning and he referred me to a Neurologist whom I also saw that morning. As per your information, he explained the 3 injuries that coujd have occurred. I am now in the 2nd stage as no feeling has returned with a constant burning and also a strange pulling sensation underneath my tongue. No taste either.
I also saw a Maxillofacial surgeon to see if I could have nerve repair surgery but he said that I could not as he would not know where the area of damage was in the nerve and I have to just wait and see in time….!
Do you have any suggestions of what can be done? Would a CT scan or MRI show where the nerve damage is and how bad it is? Couid nerve repair surgery be done even though I understand that it may only be a 50% chance of recovery, which is better than how I am now, if not healed in 6-12 months time?
I appreciate your feedback. I live in Cape Town South Africa and Mauritius.
Penny M.
Reply –
I don’t have any additional expertise or solution to offer. Between your visits to a neurologist and oral surgeon we would have to assume that you are in as good of hands as possible.
Having said that, the US government maintains an index of published medical research (PubMed).
By now you no doubt know all of the appropriate keywords to search for in regard to your condition. While searching the PubMed database you may be able to find answers to the questions you have. Better yet, possibly even the name of a researcher in your country who has a special interest in this, or information that can lead to your finding one.
Staff Dentist
Comment –
Nerve/root location and increased risk after time
We just had our oral surgeon consult to remove my daughters wisdom teeth. Upon examination of her panoramic xray from 3 years ago, the surgeon said at that time her risk for nerve damage was 1-8%. Suggested an updated x-ray and explained 3 years is a long time and most likely her risk for nerve damage has increased to an estimated 25%. That the tooth would have grown in that time. After the xray, he is shown as correct.
My question is whether her dentist should have seen this issue on the xray 3 years ago? Are dentists trained to look for this risk factor or only oral surgeons?
JB
Reply –
I’m interpreting your question in the sense that you’re disappointed that a window of opportunity of lower risk for paresthesia was missed (3 years ago).
It seems curious that 3 years ago when the X-ray was taken no suggestion for extraction was made. Yet now 3 years later with the same x-ray a decision is made to remove the tooth.
Something had to have changed. Possibly your daughter has finally entered an age group usually considered more appropriate for a wisdom tooth removal. Or possibly the tooth has drawn attention because it is now symptomatic.
Anyway, you mention how root development (growth) has now made the procedure more risky in regard to the potential for nerve trauma, and any one can understand that.
But what we’re unclear on is why the dentist should have/should not have expected that continue growth and development would have/would not have alleviated the initially identified risk.
(With continued growth, the tooth’s roots would become more fully formed, but the jaw might also grow, and the tooth continue to erupt into more normal position. If so, the complications that exist now (close relationship between tooth and nerve) might have resolved. The question being, should the dentist have anticipated that this would not occur.)
With so many variables involved (especially age and type/angle of impaction [being a determinate in how likely it was for the tooth to continue to erupt]), it really seems only your oral surgeon could give you a valid opinion on what a general dentist should have been able to reasonably surmise with your daughter’s case.
Staff Dentist
Comment –
Twitching in cheek after wisdom tooth extracted
I had an upper left molor extracted, when I came back to have the crown placed I told the doctor my left cheek was twitching, he said he’d never heard of anything related to that and dental work. It’s been a month now, and it’s still twitching, and bothersome. That’s why I started looking the condition up on the internet and found your site.
Jh
Reply –
The muscles of the cheek (you mention twitching) are operated by the buccal branch of the facial nerve (the seventh cranial nerve).
I Googled around and noticed this article “Facial nerve paralysis after dental procedure.”
In no way do I know if the situation discussed in that article applies in your case. But in reading the article you should be able to pick up enough applicable keywords to Google about your situation further, learn more, and discuss things with your dentist. Best of luck.
Staff Dentist
Comment –
Lower lip nerve damage
Nerve damage in lower right side of my lip. Its been at least 5 since I had my wisdom tooth removed. Is there a list of specialist I go to?
KB
Reply –
You state “Its been at least 5 since I had ….”. Our point is that we don’t know the time frame you’re referring to.
We’re assuming the worst and that it has been 5 months, or even years. As you probably know from consultations, or our text above, that places you in a comparatively less favorable category.
We’re assuming you’ve had consultations about your paresthesia, are frustrated, and now are seeking a practitioner who possibly has a higher level of expertise in this matter.
We know of no list like you ask about.
Phone calls to several oral surgeons in your area might reveal a single practitioner’s name (oral surgeon or neurologist) that tends to come up. Best of luck.
Staff Dentist
Comment –
NUMB
I had my upper and lower right wisdom teeth removed. After about 5 hours my novacain wasn’t wearing off and I was getting very concerned. I have paresthesia in my right side of the tongue, right side of the bottom lip and right side of my chin. I had the procedure don’t 7 days ago and I don’t feel anything getting better, if not worse. My chin feels heavy, cold in the lip and chin and sometimes the teeth. Very swollen from the procedure as well. I am very nervous my feeling will not come back. What are the symptoms like for healing? Will there be a tell tale sign that things are going back to normal? I could also see right on my xray after doing some homework that the lower wisdom tooth was directly in the nerve. Should my dentist have referred me to an oral surgeon? Or not even have taken it out? They were not bothering me, I just could not brush them so knew eventually they would be infected. Any advice would be greatly appreciated as I am very concerned about my current problem.
EJG
Reply –
We hope our late response to your comment finds your situation improving.
Paresthesia like you have is a result of some type of nerve trauma, so a return to normal will involve a healing process.
As a process, one would expect that your return of sensation would be gradual. Possibly you’ll notice some signs of renewed yet partial sensation initially, that hopefully continues on into a full recovery.
As far as a time frame, some level of early return of sensation would be a promising sign (and one that is often associated with full recovery). But everything about the healing process simply depends on the nature and extent of the trauma/injury itself (for example, slight nerve bruising vs. nerve nicking vs. severed nerve would each have a different resolution rate and different potential for full recovery).
Unfortunately, the type/extent of the injury is seldom known (in some instances a dentist might visualize a nicked or severed nerve, but usually not).
As far as your questions about your dentist and the need for, or the prudence of the extraction, it’s hard for us to reply.
The standard of care that a dentist must provide doesn’t necessarily relate to what complications have occurred but instead to the point that they must provide care at a level that a reasonably prudent practitioner would have provided under a similar set of circumstances. Only a dentist reviewing your case history could formulate an opinion to that.
There’s also the issue of informed consent. Were the risks/rewards of the procedure adequately interpreted by the practitioner and explained to you so you could make an informed decision about accepting or refusing treatment.
In regard to having the teeth out, the argument for having partially erupted teeth extracted can be a strong one. For example, you mention the potential for infection. Decay and gum disease issues can create problems too.
Best of luck toward a full recovery.
Staff Dentist
Comment –
Numb tongue
I had my right lower wisdom tooth removed on 18th of April. I lost my senses on the right side of my tongue. I can’t feel any taste, pain, and I can’t tell if it’s hot or cold. It’s been 3 months now and it didn’t get better. The only difference that I noticed is that the pressure that I feel on my tongue it reduced it’s area a little. When I was brushing my teeth, whenever I was brushing deep in the back, I use to feel needles sensation in my tongue all the way to the tip. In time, that started to happen when I was flossing on my right side. Now, I have that sensation when I try to chew on that side. Sometimes i have the sensation like that side of my tongue it’s really cold and I feel like pressing it to warm it up. I feel like drinking water all the time because it feels dry also but it doesn’t help. I started taking vitamins b6-12 etc because someone told me that it may help with the recovery. I’m honestly desperate. I can’t take it anymore it’s horrible. It’s harder to talk and stuff. What can I do? I’ve been to my dentist many times and she tested my tongue because she couldn’t believe that I really don’t feel any pain. She said that it’s imposibile to not recover. I read a lot of stuff, everybody is saying how rarely this happens to be permanent, but there are so many ppl heeding this problem for years now. Please, help me with info and anything!
Ligia F
Reply –
What seems salient about your narrative is that instead of “just” dealing with the loss of sensation, what you feel is altered sensation, much of which is painful, and instead of dimenishing with time, now 3 months out you notice the effect has expanded.
There is no question that no one knows how your case will ultimately turn out. But it does seem clear that your case isn’t taking the course that is most common, and it hasn’t taken any turns that seem especially positive.
The current recommendation is “wait and see,” which may be the only alternative available. But if a case is difficult or non-standard, it seems reasonable that the patient might seek the highest level of expertise available on the subject.
We would discuss with your dentist about a referral to an oral surgeon. It would be expected that they would have more experience with patients experiencing this difficulty. Know more about current treatment modalities for the problem, whether they themselves could provide that service or in turn would need to refer. They might have an opinion about when it makes sense to consider further steps, like nerve surgery, in light of how the patient’s case is currently progressing.
We don’t know that they could provide a solution, or that further steps are indicated. But a consultation seems harmless enough considering the distress this experience is causing you. Best of luck.
Staff Dentist
Comment –
Numb and high pain
So a dentist removed two bad teeth, at first i thought the pain was the result of bit of old tooth left behind.
I went back twice, they seen nothing.
The numbness started, the pain got worse and i have phlegm in throat.
Since then, about 2 weeks later i went into hospital to have the rest of my teeth out.
8 weeks on, pain still there, visit ae at hospital they did xray, discharged with antibiotics and mouth spray
Pain continues, what to do?
John
Reply –
The way we interpret your narrative, your numbness (paresthesia) didn’t present itself immediately following your extractions but instead some days/weeks? later.
That’s rare and substantially different than what usually happens with dental patients (where the numbness has an immediate temporal relationship to an extraction, root canal, injection or implant procedure). (We’ve linked to an article below that discusses a delayed type of situation.)
Due to the unusual nature of your case, we would think that a general dentist would have little insight to offer. (From your narrative, it seems that yours is no longer involved anyway.)
We can imagine how treatment at a hospital emergency room would be geared more toward immediate patient stabilization and comfort (hence the antibiotic and spray) as opposed to rigorous evaluation and differential diagnosis.
You mention that some of your teeth were taken out in a hospital setting. We’re guessing that those services were performed by an oral surgeon. We would think that your best chances of finding a diagnosis and solution starts with them.
They know your case and original symptoms. And they have added insight about your case from providing you with treatment.
As a specialist, they should be knowledgeable enough to know what about your case makes sense from a dental vs. medical perspective, and can either suggest further treatment ideas or know what type of medical doctor to refer you to for further evaluation.
Good luck.
Staff Dentist
Comment –
Wisdom teeth extraction and tongue sensitivity
My 17yr old daughter had all 4 wisdom teeth extracted on 2-15-2017. Within 2 weeks of extraction she noticed her tongue had numbness directly down the center of her tongue. The right side of her tongue did not having feeling for quite a long time, approx.6mths. We went back to the oral surgeon monthly to determine if any sensation was coming back. She does have some sensation, but not much, but now she is complaining a lot that her right side of the tongue has a burning feeling and she is constantly biting her tongue when eating. She is very frustrated and now that it has been about 18 months since the extractions, I don’t know what to do? What recourse do I have? Is there a special oral surgeon I should take her to? Any advice would be greatly appreciated.
AZ
Reply –
You state that your daughter’s procedure was performed but rather than immediately postoperatively, her symptoms developed over the next 1 to 2 weeks (that’s known but rare).
(FYI: In Googling, we ran across this paper about delayed dental paresthesia.)
You also describe that the center of her tongue was numb initially. The tongue is innervated by the left and right Lingual nerves, so that symptom (just the center) seems strange.
Now 1.5 years later, her case is not resolved, and is changing in nature for the worse.
—
At 1.5 years, her condition lies beyond the expected time frame for paresthesia recovery.
Her symptoms are in transition and we don’t know how to interpret that. But considering their nature, that course doesn’t seem all that positive.
While we know very little about delayed paresthesia, the paper linked to above suggests that it typically resolves favorably, but of course it hasn’t.
The symptoms she has significantly affect her life.
—
We’re not clear if you still see the oral surgeon monthly. We’re assuming not.
We would simply contact them, explain to them the current state of affairs, and ask them what the next step is.
As an oral surgeon, we would think they would have little to offer other than a referral. We would anticipate that referral would be to a neurologist or neurosurgeon for evaluation.
We have no learned opinion about specifically what solution they might suggest, if a solution or reasonable attempt of some sort (like nerve repair) exists at all.But considering your daughter’s case history and current status, we hardly see how fresh viewpoint from a new direction wouldn’t be a positive and logical next step. Good luck.
Staff Dentist
Comment –
Numbness of right side of tongue
Hi, I had four wisdom teeth extracted in July 2017 ( a year ago exactly) and i had almost 90% loss of sensation in my right side of tongue with extremely uncomfortable tingling and burning feelings, and the Oral Surgeon said that about 2 mm of apex of the mesial root of lower right molar was broken and left in place which I dunno if it was related to my symptoms.
Now after 12 months, i approximate improvement in the range of 60-70% but with still ongoing burning feeling which is really uncomfortable.
Do you believe waiting for few more months may result in satisfactory recovery or I should start consulting nerve repair specialists? And do you know any specific clinic that may provide surgical repair?
Based on my internet research, some say surgical approach should be taken within 6 months of injury otherwise it will be late. Thanks a lot.
Nathan
Reply –
If it’s your tongue that displays symptoms, the root tip probably isn’t a directly associated issue.
The tongue is innervated by the lingual nerve. This nerve runs through the soft tissues (not inside the bone but along its surface) in the area of the third molar. The trauma it received was most likely related to the act of incising and reflecting back these tissues as a part of accessing your wisdom tooth.
We’re not going to have any special expertise to offer, nor clinicians to suggest. We think your questions are best directed to your oral surgeon, someone who should be expert on the subject, has a familiarity with your case and possibly has a referral to someone in your area in mind if they think that’s indicated.
Your narrative seems to imply that improvement is still progressing. But you don’t really say how the burning issue has changed (better, no different). Contact your oral surgeon and discuss those issues with them and let them advise you on what seems a reasonable plan. Good luck.
Staff Dentist
Comment –
Nerve touching tooth
My dentist recommended to have my impacted bottom wisdom tooth removed. He also said the X-ray was showing that it seemed the tooth was touching a nerve. He said he wasn’t sure because it was only a 2D picture, that it could be in front of or behind the tooth. I am 28 years old and have no symptoms and I’m scared of nerve damage. Should I proceed with my extraction even if I haven no symptoms.
Thank you
Amanda R
Reply –
Of course we really can’t answer your question, however you might read through our pages about reasons to and not to have wisdom teeth removed. Some of what we state there may correlate with what you know about your situation and can help you decide what makes an acceptable plan for you.
Your dentist is right in the sense that their x-ray is a 2-dimensional picture of you, a 3-dimensional object. And as such, the precise relationship between your tooth and the nearby nerve is an unknown.
As this page mentions, nowadays in dentistry the use of 3-D imaging (cone beam computed tomography) is becoming more and more common. And via it’s use, a better understanding of the tooth-nerve relationship can most likely be determined.
Due to the expense, it’s more common for oral surgeons to have this type of equipment in their office. With cases where a question exists, that might be a reason to be referred to one.
Of course, dentists have been using 2-D imaging for this type of diagnosis for well over a half century. And generally it’s considered that those who are expert in reading them can formulate a fairly accurate opinion about what exists (research studies confirm this). We would think experience matters in being able to do so.
Staff Dentist
Comment –
Nerve pain after wisdom tooth extraction
Hi, I had a lower wisdom tooth removed two weeks ago and have been in severe pain – like toothache in jaw and neck, radiating to shoulder. I’ve been back to my dentist twice and eventually went to another dentist. They think it might be nerve damage and that it will eventually go away. The pain is very bad at times – is there any treatment to help?
Fh
Reply –
We hope our late reply finds your recovery progressing.
We’ve added content to our treatment section above. Possibly there is an approach mentioned there that can be discussed with your dentist.
In passing, we’ll mention that the incident rate of experiencing paresthesia after lower wisdom tooth removal has been estimated, at the very most, to lie on the order of 8%.
And we find it hard to believe that very many general dentists even come close to averaging one lower wisdom tooth extraction per day, with very few of those being impacted cases (the type of tooth extraction most associated with paresthesia).
Our point being, consider the idea that an oral surgeon would have much more familiarity with this complication than the average general dentist. As such, they would know more about current treatment modalities for it, and when those might be indicated.
Staff Dentist
Comment –
38 year old
Hello. My top right wisdom tooth grew out like a normal tooth. Just recently while eating the tooth craked. I visited my local dentist because their was a sharp edge rubbing against my gum. They grinded it down and said that I need to extract it and at an oral surgeon they recommended. They also did a panoramic and I have all 4 wisdom tooth. 1st being the top right that craked. 2nd top is slightly beginning to come out of the gum. 3rd is button and is horizontal with 3mm distal probing and the 4th is buttom and is horizontal with 11mm distal probing. My question is should I remove all 4 using coronectomy techniques. I know the 1st need to be removal for sure, the surgone said he will be use coronectomy because of the nerours attached to it. Also I thinking also of doing the 4th one. Any suggestions ?
Aaron
Reply –
For others reading, a coronectomy refers to a procedure where only the crown (top) portion of a tooth is removed. After the crown has been sectioned off, the roots of the tooth are left in place. This is a procedure most associated with impacted wisdom teeth. And usually just lower ones whose roots have a close proximity to the mandibular nerve.
The general idea is that the removal of the tooth’s crown resolves issues its positioning was causing (or had potential to cause) such as pericoronitis, damage to neighboring teeth, gum disease, etc….
The roots are left in place because there is fear that removing them will traumatize the adjacent nerve, resulting in paresthesia (persistent numbness, like discussed on this page).
We’re thinking there may be a communication problem here and anticipate that your oral surgeon has only recommended the coronectomy for your lower wisdom teeth.
We’d be unclear as to the purpose of this procedure for the upper ones. You describe them one already being erupted and the other starting to (so they should both be fairly routine extractions). You mention the potential for nerve damage but paresthesia associated with removing upper wisdom teeth is not common.
Staff Dentist
Comment –
Getting wisdom teeth extracted
Hi i am 24 and i’m getting my wisdom teeth extracted an the bottom left tooth is grown in side ways instead of up the other bottom right right tooth is impacted and the one top left is flat surface all four are infected and they have to be extracted in a hospital setting due to my medical issues but im really scared about getting a damaged nerve and i was wondering how likely is that, is it pretty rare?
Because I don’t know how i would live if a nerve got damaged. Im very scared as is and i will be under general anesthesia.
Jamez
Reply –
One would only imagine that you’ll do great with your procedure.
You mention the term “hospital setting.”
That implies, an oral surgeon will perform your work (as opposed to a less experienced and trained general dentist).
You also mention having “general anesthesia.” That means patient cooperation will not be a factor and your surgeon will be able to solely focus on the process of removing your tooth as expertly as possible.
While always a possibility, you seem to have as many factors stacked in your favor as possible. Good luck.
Up above on this page there is a section that contains statistics about how often paresthesia occurs.
Staff Dentist
Comment –
Horizontal wisdom tooth removal
Tomorrow I am scheduled for the surgery required to remove my horizontally grew wisdom tooth (down, right). I am 27 years old. At the 3d scan I took 2 days ago it showed that the roots of the tooth are ‘hooked’ to the nerve and the doctor had said that there are chances in the moment they will pull the tooth out for the nerve to be damaged. I will experience numbness for hours, or days, or weeks, or months or it the nerve will never fully recover and the numbness will stick forever. We won’t know until it is done..
i am quite concerned and I am trying to make a list of questions to ask the doctor before the surgery. Maybe you could give me some ideas, please.
Thank you!
Ana
Reply –
Good luck tomorrow.
We’d like to think that possibly what your dentist has stated is simply very thorough “informed consent” information, to the point of overstating what they actually anticipate is most likely to happen. Hopefully your actual level of risk is substantially less than what you currently imagine.
—
Where the potential for complications with paresthesia are comparatively higher, we would make sure we were in the most capable hands possible, meaning an oral surgeon as opposed to a general dentist.
Based on your mention of a “3d scan” (a type of imaging that most general dentists don’t have in their office), we’re assuming you have that issue covered.
—
There should be clear reasons why the tooth needs to be removed, including an explanation of why the issues associated with leaving it exceeds the expected risk for permanent nerve damage. (We have pages that discuss general reasons why wisdom teeth should be extraced and others that may not be such valid reasons.)
—
In terms of questions to ask about how the procedure will be performed to help prevent nerve trauma from occurring, only your doctor can determine the approach that’s best.
For a horizontally positioned tooth, we would imagine some degree of sectioning would be planned for (see above on this page). That would be positive to know because usually that means the tooth can be removed relatively less traumatically.
—
Generally, we would just focus on the fact that the tooth has good reason to be removed. That we are in the hands of a highly trained and skilled practitioner. And that you and they want the exact same thing, the most uneventful extraction process for you possible. Once again, good luck.
Staff Dentist
Comment –
Complications
Hi, I had wisdom teeth removal October 2019 using Local Anesthesia. I believe I experienced the shock which you mentioned while receiving one of the injections. This is now February 2020, I have numbness on my lip and chin area on the left side. I believe the numb area is getting smaller than when I first had the surgery. But the strange thing is when drink cold water I feel it “rushing down” on this side like if it was outside of my mouth
S.n.
Reply –
Only as speculation, one might hope that the nerve that innervates this region is in the process of recovering but is still immature and therefore doesn’t yet respond appropriately when stimulated. Or possibly during the healing process some type of nerve fiber reorganization has occurred that has resulted in the referred sensation you experience. Hopefully your condition will continue to progress and ultimately resolve in your favor.
Staff Dentist
Comment –
Loss of sensation in the lips after 20 tooth extraction
Hello, it has been 2 days since I had my teeth removed and I am very worried about the numbness in my lips. Is there any chance that it becomes permanent when you look at the x-ray photo? I would be glad if you answer. I could not find the place to send a photo. Can you give me a phone number that I can send from WhatsApp. 🙁
Ilayda
Reply –
The traumatized nerve fibers are “soft tissues” as opposed to hard, like teeth and bone, and as such nothing informative about their current condition will be evident on an x-ray.
With tooth #20, and the lip numbness you describe (lower left? lip, across to the midline?), one would have to assume that the traumatized nerve is the “inferior alveolar nerve,” possibly at a point where it comes out of the “mental foramen” (Google that for a picture). That’s the point were the nerve exits the jawbone and runs to the lip.
With a routine extraction process, possibly some type of compression of the bone has aggravated the nerve. If the extraction was more surgical in nature (like a gum flap was created), the likelihood of the nerve having been severed might be considered more likely.
With the former, the continuity of the nerve is still intact, and possibly recovery on its own more likely. If the nerve has been severed, some type of repair might be attempted at some point. But only doctors at your end could determine if and when that is indicated. Good luck. Hopefully your situation will resolve promptly on its own.
Staff Dentist
Comment –
Possible paresthesia
Hi, I don’t know the name of the tooth but I had the third one from the back at the top right removed yesterday and the anesthetic took a while to wear off, and I have been to sleep and got up and it’s still numb on the right side of my tongue. Is there a time frame I should wait for it to go away before talking to my dentist again? I have another appointment for a filling next Friday if that helps. Thank you! 🙁
Lissa
Reply –
You report that the tooth removed was “the third one from the back at the top right”. Since some people have wisdom teeth and others don’t, precisely which tooth has been removed would still be in question. However, it was either a 1st upper molar (a large 3-rooted tooth), or else a upper 2nd premolar (a much smaller tooth).
You also report “still numb on the right side of my tongue”. That symptom would involve some type of trauma to the Lingual nerve.
The lingual nerve branches off of the Mandibular nerve at a level up around where your jaw hinges on your skull. And then runs through the soft tissues that cover the inside of your jawbone, and then finally to the tongue. (this picture shows this well)
A difficulty in understanding your case is that none of that area where the nerve runs is close to the tooth you have had taken out. So how did the nerve get traumatized?
As an explanation, dentists sometimes use a “Gow Gates” injection to numb teeth and tissues up. And this injection is given precisely in the area where the lingual nerve branches off of the mandibular nerve.
So, one might hypothesize, that an injection is the source of the trauma and your symptoms. (So reread this page focusing on that cause.)
You should always feel free to let your dentist’s office know you have experienced a complication. And with this, for example, they may want to set aside a few extra moments during your Friday appointment to test and document (map) the extent of where the numbness lies, so future improvements can be compared.
Good luck on this. Hopefully this will be short lived.
Staff Dentist
Comment –
Persistent numbness.
I had my bottom right wisdom tooth removed 1.5 years ago which was horizontal and my doctor let me know about the complications such as numbness on the lips. Unfortunately I lost my sensation not only on the right side of my lip but also chin. I took B12 pills for 6 months according to my doctor’s advice. Then took B12 pills for a few additional months and then quit since I had no hope that my sensation will come back. Now, I am curious again whether after all this time, a recovery can be possible? Should I start B12 again? Would that help maybe not fully but any?
Thank you,
Pinar
Reply –
This section of this page discusses that the outlook for cases that don’t resolve within 8 weeks typically isn’t very favorable. And here’s a paper that discusses the use Vitamin B12 in aiding neural regeneration (note that they are looking for improvement over a very short time frame).
At this point in time, one might anticipate that as much healing/regeneration that will/can take place has, and that the possibility of a surgical repair might be considered. Best of luck.
Staff Dentist