Risks and complications of wisdom tooth extractions.
Complications of wisdom tooth extraction.
No surgical procedure is without risks. And in the case of wisdom tooth removal, there are a number of known post-surgical complications that patients tend to experience. This page provides an overview of the more common ones that are likely to occur.
What are the common complications associated with wisdom tooth extraction?
Here’s a listing of the most frequently occurring postoperative conditions, along with their estimated incidence rate:
► Postoperative surgical site infection – As opposed to routine surgical swelling What’s normal? that peaks 2 to 3 days following an extraction, swelling that persists, or first appears outside of this time frame, is likely due to infection.
Incidence rate: 0.8% to 4.2% of cases.
► Bleeding and hemorrhage – While all extractions sites display some level of postoperative bleeding What’s normal?, some wisdom tooth extractions are accompanied by clinically significant (excessive) levels of bleeding, either during or after the patient’s procedure.
Incidence rate: 0.2% to 5.8% of cases.
4 most frequent post-extraction complications. (Percent of cases.)
- Dry socket – 0.3% to 26%
- Nerve damage. / Paresthesia – 0.4% to 8.4%
- Bleeding / Hemorrhage – 0.2% to 5.8%
- Surgical site infection – 0.8% to 4.2%
► Dry Socket (Alveolar osteitis) – This is a painful condition that involves delayed wound healing that first becomes noticeable a few days after the patient’s surgery.
Incidence rate: 0.3% to 26% of cases.
► Paresthesia (nerve damage) – Nerve damage sustained during the extraction of wisdom teeth can lead to altered or loss of sensation of soft tissues (lip, chin, tongue, floor of mouth).
Incidence rate: 0.4% to 8.4% of cases. (Blondeau)
► Damage to adjacent teeth – The instruments used during the extraction process may put neighboring teeth at risk.
Incidence rate: 0.3% to 0.4% of cases.
► Jawbone fracture – This is a possibility with extractions on either (upper or lower) jawbone.
Incidence rate: Up to 0.6% of cases.
► Displacement of the wisdom tooth – The forces used in an attempt to remove a tooth may instead displace it.
Incidence rate: Infrequent but possible.
► Wisdom tooth aspiration – Loss of control of an extracted tooth may result in it being swallowed and possibly entering the patient’s airway.
Incidence rate: Infrequent but possible.
► Sinus communications – Extracting upper wisdom teeth may result in problematic openings into the patient’s sinuses.
Incidence rate: Up to 0.25% of cases.
► Jaw function complications – A patient’s temporomandibular joint (jaw joint) or the muscles that operate it may be aggravated by the extraction process.
Incidence rate: Debated.
▲ Section references – Blondeau, Blouloux
Postoperative surgical site infection.
The development of a bacterial infection following the extraction of a wisdom tooth has been estimated to lie on the order of 0.8% to 4.2% of cases (Bouloux). However, with lower wisdom tooth extractions this number has been suggested to be as high as 27% (Susarla).
Signs and symptoms.
Infections can develop in the early (within days) or late (weeks later) postoperative period. By far they are most commonly associated with the removal of mandibular (lower) third molars.
As opposed to routine surgical swelling that peaks 2 to 3 days after an extraction and then begins to subside, postoperative surgical site infection can be expected to persist beyond this time frame, or develop completely outside of it.
The swelling may be accompanied by increasing pain, pus drainage from the wound, fever and chills.
Risk factors.
A number of factors have been identified as having an association with the development of post-surgical infection. They include advanced age, the types of bacteria living in the operative site before the procedure and their status, the surgeon’s clinical experience and the type of surgical facility (office vs. hospital).
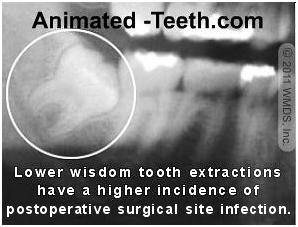
X-ray of impacted mandibular 3rd molar.
- Tooth location – The incidence rate of post-surgical infections is much greater with lower vs. upper third molars (see statistics above).
- Surgery duration – The development of infection is more common with extraction procedures that are comparatively more involved.
This includes those that require bone removal and tooth sectioning Surgical tooth extractions. (steps that are often needed to remove impacted wisdom teeth).
Prevention.
It’s common for a dentist to utilize preoperative antibiotics with a patient as a preventive measure, especially when the procedure planned involves the removal of impacted lower third molars.
The dentist or oral surgeon has a number of options in how the medication is administered.
- It’s generally considered most advantageous if it’s given prior to the patient’s surgical procedure.
- Oral antibiotics are typically given at least 1 hour prior to the patient’s surgery. As an alternative, the dentist might choose to administer the medication systemically (I.V.) at the start of the patient’s procedure, or topically (applied directly to the wound) after their tooth has been removed.
- With some regimens, the patient will be asked to continue taking oral antibiotics for some days following their procedure
- A decision about the need for antibiotics is only made by the dentist after evaluating their patient. Not all wisdom tooth extraction cases require them.
The current trend seems to be one where pre-treatment coverage is used less frequently. Over usage promotes bacterial drug resistance, and places the patient at risk for medication-related complications.
Treatment.
Postoperative surgical site infections can be serious events. And if timely treatment is not initiated and the infection is allowed to spread into the tissues of the head and neck, even life-threatening.
▲ Section references – Susarla, Marciani, Blondeau, Bouloux
Bleeding and hemorrhage.
All extraction procedures will be accompanied by bleeding from the surgical site. And in most cases, this type of bleeding is easily controlled Instructions..
Beyond what’s expected and considered normal, some wisdom tooth extractions will be plagued by the complication of excessive (“clinically significant”) bleeding.
Incident rates.
- Studies have reported rates of unexpected or prolonged significant bleeding as a complication of third molar extractions ranging from 0.2% to 5.8%.
- It seems likely that the true number probably lies in the area of 0.7%, with many of these cases involving bleeding that occurred during the patient’s procedure as opposed to following it.
- Excessive hemorrhage is more likely associated with the removal of lower third molars as opposed to upper ones.
▲ Section references – Blouloux
Prevention.
While many of the issues associated with bleeding complications lie beyond the patient’s control, they do play a role in helping to avoid them.
- A number of medical issues View the list. are known to affect a person’s blood clotting cascade. Additionally, the medications View the list. a person takes may have an effect too. Additionally, local conditions surrounding your tooth can also impact the amount of bleeding that occurs.
Discovering all of these issues and making a determination about how they need to be managed is a part of the purpose of a patient’s pre-treatment clinical examination and history taking, so give your dentist your full cooperation.
- The patient’s ability/willingness to follow their dentist’s postoperative instructions can play an immense role in how easily their postoperative bleeding is controlled.
There should be two sets of directions, one for the first 24 hours post-op Instructions list., another for the days following Instructions list.. (Use our links for information about the type of directions these instructions typically include.)
Treatment.
In all cases where you suspect that complications with bleeding exist, you should contact your dentist immediately. Until that moment when they are able to take over the management of your care, the use of gauze, or a tea bag, and pressure Directions may help to control your situation.
Dry Sockets
What are they? What causes them?
Note: We have expanded our coverage of this complication to several pages. It begins here: What are dry sockets?
Dry sockets (alveolar osteitis) are a painful, foul-smelling and tasting postoperative complication that typically becomes apparent 3 or 4 days following the patient’s extraction.
- Their formation is associated with situations where either an adequate blood clot has failed to form in the extracted tooth’s socket, or else the one that did form has been lost.
- Since the formation of a clot is an important part of the healing process, the healing of the extraction site is delayed and disrupted.
Signs and symptoms.
- A dull, often throbbing, pain that doesn’t first appear until three or four days after the tooth has been extracted.
- The pain can be moderate to quite severe.
- The socket typically has a foul odor or taste coming from it.
How likely is it that a person will develop a dry socket?
Although there are risk factors View the list. that may predispose a dental patient to the formation of a dry socket, knowing who will actually develop one is totally unpredictable.
Rules of thumb.
- There is a greater likelihood of their formation with the extraction of lower wisdom teeth, as opposed to upper ones.
- Their incidence is typically greater with the removal of impacted wisdom teeth, as opposed to non-surgical extractions.
Research – Incident rates.
A literature review performed by Blondeau suggested an incidence rate for dry sockets following third molar extractions ranged between 5% and 10%.
This should be viewed in light of Bui’s review of dental literature that suggested an incidence range of 1% to 3% for all tooth extractions as a whole.
Bui cited the findings of a study that reported a dry socket incidence rate as high as 30% for impacted lower wisdom teeth. Chuang found the incidence of “inflammatory postoperative complications” to be more than twice as high when full-bony wisdom teeth were removed, as compared to soft-tissue third molar impactions.
What is the treatment for dry sockets?
▲ Section references – Bui, Chuang, Blondeau
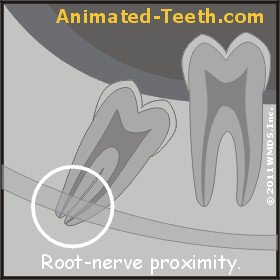
With some tooth extractions, nerve trauma is a possibility.
Paresthesia (nerve damage).
What is it? / Signs and symptoms. / Incidence.
Blondeau suggests that published literature reports an incidence rate of 0.4% to 8.4% for this complication.
Prevention.
In terms of a preventive measure you can take, hoping to avoid the complication of paresthesia is one reason why dentists suggest that wisdom teeth should be removed when a patient is still comparatively young. Best age for wisdom tooth removal.
That’s because as people age on through their twenties, the roots of their wisdom teeth continue to form and develop. And as this occurs, these teeth can become significantly more difficult to extract without disturbing surrounding tissues (like associated nerve bundles).
In general, the incidence of nerve damage associated with wisdom tooth removal for people over the age of 35 years runs relatively high, whereas with teenagers it’s rare. So if the need for the removal of your wisdom teeth is diagnosed in the more favorable time window, following through with your dentist’s recommendation makes a good choice.
For more complete coverage of this topic –
▲ Section references – Blondeau
Damage to adjacent teeth.
While never the dentist’s intention, it’s possible that damage to the tooth directly adjacent to a wisdom tooth (a 2nd molar) will be damaged during its extraction process.
Causes.
In most cases, the damage is caused by pressure placed on them by the instruments used to remove the wisdom tooth (a dental elevator would be a common culprit How extraction instruments are used.).
That’s not the way extraction instruments are intended to be used. But in locations where access is difficult and visibility low (like the places in the mouth where 3rd molars are located), this complication is possible.
Incident rates.
▲ Section references – Blondeau
Jawbone fracture.
The mandibular (lower) jaw.
Fracture of the lower jaw during wisdom tooth removal is rare. Reports in published literature place the incidence rate at less than 0.005% of cases. (Blondeau)
Causes.
Changes or conditions associated with the jawbone are often a predisposing factor. These include osteoporosis, jawbone atrophy, or the association of a cyst or tumor with the wisdom tooth. Each of these can have the effect of weakening the jaws structural integrity.
While the fracture may occur during the patient’s treatment (a status that’s not always easy to identify), the jaw’s weakened state that exists after its procedure has been completed is also a concern. Many fractures are “late” ones, occurring some days or weeks following the patient’s surgery. Usually in association with eating.
The maxillary (upper) jawbone.
Causes.
As compared to the lower jaw, the bone making up the upper jaw is “softer” (less dense). Additionally, it houses portions of the nasal sinus (thus it is not just solid bone). And by nature of its anatomy, that portion of it that houses the wisdom teeth (the maxillary tuberosity) is relatively unsupported bone.
As such, it’s possible that a portion of the tuberosity will fracture during a wisdom tooth’s removal, often coming off still attached to the tooth itself.
Incidence rates.
Dental literature suggests that this complication takes place with 0.6% of cases. (Blondeau)
Treatment.
▲ Section references – Blondeau
Wisdom tooth displacement.
This complication refers to the situation where control of the wisdom tooth being removed is lost and it enters an adjacent portion of the patient’s body. The entire tooth might be displaced or some fragment of it (like in the case of sectioned or broken teeth).
Causes.
It’s easy enough to suggest that the tooth’s displacement is associated with using a level of force greater than its supporting tissues can withstand. But to the dentist’s defense, determining what amount of supporting tissues exist, and therefore what level of pressure is appropriate to use, can be exceedingly difficult to determine.
As an example, the thickness of bone that encases an upper wisdom tooth’s roots and also serves as the floor of the adjacent sinus may be just paper-thin.
Incidence rates.
A paper by Blondeau states that the complication of wisdom tooth displacement is seldom reported in dental literature and as such gives no estimate of its occurrence.
Treatment.
▲ Section references – Blondeau
Wisdom tooth aspiration.
This complication involves the situation where control of the removed tooth is lost and swallowed by the patient, and subsequently enters their airway (passageway to the lungs).
Causes / Prevention.
This type of event is usually prevented by way of placing gauze across the rear-most portion of the patient’s mouth. But events such as coughing or gagging may result in this complication.
Treatment.
While a description lies beyond the scope of this page, the location of the tooth must be identified and if discovered to be in the patient’s airway, it must be removed.
Incidence rate.
This is a possible but rare event.
Sinus communications.
As mentioned above, it’s possible that the bone that both encases an upper wisdom tooth’s roots and serves as the floor of the adjacent sinus is just paper-thin. And as such, it’s possible for this fragile bone to be damaged or lost during the tooth’s extraction process.
Incidence rates.
This complication is reported to involve up to 0.25% of cases (Blondeau). But in reality, some minor level of disturbance likely occurs much more frequently than that but heals uneventfully and unnoticed.
Treatment.
In many, if not most cases, the normal healing process that follows a tooth’s removal will simply and uneventfully repair the damage that has occurred.
However, in those cases where this does not occur on its own and an opening remains through which air and fluids can pass (between the oral cavity and sinus, referred to as an oro-antral communication), a second surgical procedure will be required to block off this passageway so normal healing can occur.
A dentist will test for the presence of a communication after removing a tooth by way of holding their patient’s nose shut and then having them gently blow air into their nose. If bubbles are noticed in the tooth’s socket, a communication exists.
▲ Section references – Blondeau
Jaw movement complications.
It’s suggested that the patient’s need to remain wide open for the extended period of time required for their wisdom tooth procedure can aggravate their tempromandibular joint (TMJ, jaw joint). Possibly the lateral forces exerted while working a lower one loose How extraction instruments are used. may contribute too. However, the extent to which this actually occurs is debated.
These same activities may also contribute to a complication termed trismus (spasm of the muscles that operate the jaw). Other possible causes may include other aspects of the procedure, including receiving injections.
Treatment.
In most cases, jaw issues will tend to resolve on their own, although it may take several days or even a few weeks for them to do so. Even so, a patient should contact their dentist to see what solutions they recommend (possibly as an aid in speeding up the healing process). In some cases their direct evaluation may be needed.
Page references sources:
Blondeau F, et al. Extraction of impacted mandibular third molars: postoperative complications and their risk factors.
Bouloux GF, et al. Complications of third molar surgery.
Bui CH, et al. Types, Frequencies, and Risk Factors for Complications After Third Molar Extraction.
Chuang SK, et al. Risk factors for inflammatory complications following third molar surgery in adults.
Marciani RD. Complications of Third Molar Surgery an Their Management.
Susarla SM, et al. Do antibiotics reduce the frequency of surgical site infections after impacted mandibular third molar surgery?
All reference sources for topic Wisdom Teeth.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Wisdom tooth extraction infection
Recently I had my wisdom tooth pulled out on the lower side of my jaw. Shortly after I developed an infection that I had to have my dentist scrape out. It has now been 3 weeks after and I still have swelling. Although the swelling has gone down it has now seemed to stay in the current state it is in. I had to check up with the dentist and he prescribed me more penicillin and said to see him back in 6 weeks. I’m wondering if this is normal that the swelling hasn’t gone down completely yet. The pain is not as severe as before I had the infection but I do notice a tender feeling on the back of the teeth when chewing food. Any help will be greatly appreciated thank you
Rip
Reply –
Here’s a link to an article that discusses osteomyelitis, which is an infection of the bone that sometimes occurs as a postoperative complication of tooth extractions, especially lower 3rd molars.
We chose this article only because it contains some general terms and specifics that you can familiarize yourself with and then Google further about. We doubt that the outcome of the case itself correlates to your situation to any significant degree.
Good luck. Hopefully this will resolve quickly and uneventfully for you.
Staff Dentist